In this month’s alert
What are Alcohol Care Teams? – podcast feature
[Moving forward, we will be publishing the podcast separately from, but alongside, the newsletter, to improve discoverability on podcast platforms]
On this month’s podcast we spoke to Professor Julia Sinclair and Arlene Copeland about Alcohol Care Teams – the small but vital hospital teams supporting patients with complex alcohol problems.
They explained how ACTs not only manage alcohol withdrawal, but also build trust with vulnerable patients, advocate across departments, and link people to the wider support they need. Despite clear evidence they improve care and reduce costs, many teams now face closure as funding dries up.
We also explored stigma, the misunderstanding of addiction in healthcare, and what’s needed to secure these essential services for the future.
As Professor Sinclair puts it:
This is about working with some of the most vulnerable people with the greatest needs.
You will receive the podcast in your inbox and links can also be found on our website here.
10 Year Health Plan fails to include most effective policies to reduce alcohol harm

The much anticipated 10 Year Health Plan for England was published on 03 July. Regarding alcohol, it failed to include any of the three most effective policies to reduce harm (on pricing, availability, and marketing). Instead, there are two key alcohol policies:
- Introduce mandatory labelling requirements for alcoholic drinks to display consistent nutritional information and health warning messages, to allow consumers to make more informed, healthier choices.
- Support the growth of the zero and low alcohol sector, by changing the upper threshold of zero drinks from 0.05% to 0.5%. Alongside this they will restrict these drinks so they cannot be sold to under 18s.
The government will also support “innovative community-level innovations where they have shown promise in reducing alcohol harm” such as peer-led support groups, coaching, and mutual aid networks.
Alcohol charities responded with disappointment, particularly as minimum unit pricing (MUP) and partial advertising bans had reportedly been in the first draft but been stripped out due to industry lobbying and political decisions from No.10.
Professor Sir Ian Gilmore of the AHA said:
For a moment, it looked as though the government might finally be ready to confront the toll alcohol takes on our society. Instead, that opportunity has been squandered. This is not just a missed opportunity – it is a dereliction of duty.
Most notably, Minimum Unit Pricing – a measure proven to reduce alcohol deaths and cut health inequalities – was reportedly included in earlier drafts but has now been omitted. If true, this is a grave mistake.
IAS’s Jem Roberts responded that:
It’s frankly embarrassing to launch a ‘prevention’ plan that ignores the most effective ways to prevent alcohol harm. Deaths are at their highest level in decades and have risen over 40% in recent years – yet the government has dodged proven policies like minimum unit pricing, marketing restrictions, and availability controls.
We support clearer labelling, but it must be developed independently. The alcohol industry has kept people in the dark for years – and it has no place writing public health policy.
On Bluesky, Professor Colin Angus of the University of Sheffield said:
We don’t really have any evidence to support the idea that increasing the no/low market actually reduces alcohol consumption. All of which leaves a rather bad taste in the mouth. The 10 year plan claims that it will help tackle alcohol harm. While the labelling policies are sensible enough, there is little reason to believe that the actions in the plan will make any difference at all to record levels of alcohol harms.
We’ve spent the last year listening to the government say sensible, if generic, things about being committed to a prevention agenda. We’re seeing today that this, from the perspective of alcohol, was all mouth and no trousers whatsoever.
Matt Lambert of the industry trade body the Portman Group said he: “doesn’t believe there is a case for wider health warning labels [which] may be disproportionate when overall alcohol consumption is falling and the majority of people already drink within the Chief Medical Officer’s low-risk guidance. As the alcohol industry regulatory body for marketing, we ensure that adults who choose to drink have actionable and evidence-based information to make informed choices.”
Miles Beale of the Wine and Spirit Trade Association said the trade body welcomed “the Government’s commitment to tackling harmful consumption of alcohol. The drinks industry already supports the UK’s highly successful voluntary labelling scheme and is keen to work closely with Government on this agenda.”
Both welcomed the government’s promise to support the zero and low alcohol sector.
A consultation on labelling is expected to be launched in the coming months.
In The Times IAS welcomed the promise on labels but warned that “industry will push for weak, hard-to-read labels, or QR codes few people will ever scan — anything to delay or dilute the policy.”
More generally, the plan received mixed responses, with some welcoming it as having radical ideas if implemented effectively. However, the King’s Fund’s Sarah Woolnough responded that there was:
Nowhere near enough detail about how it will be implemented. Without this detail it is hard to judge how the ambitions written on the page will make a difference to the reality of the care we receive over the next few years.
On alcohol, The Kings Fund stated that:
It is truly disappointing that the government has ducked out of anything that will shift and target harmful alcohol consumption.
In mid-July, Health Secretary Wes Streeting gave evidence to the Health and Social Care Select Committee and was asked why MUP hadn’t been included in the plan. Streeting responded that minimum unit pricing is not something the government has chosen to proceed with at this time. Instead, he said they are proposing to give the consumer more health information. He also said more needs to be done on ‘problem drinking’, since 4% of people drink 30% of all alcohol consumed.
Ireland’s health warning labels delayed until 2028
The Irish Government has confirmed that it will delay the introduction of health warnings on alcohol labels from 2026 to 2028.
In recent months there have been many reports that a delay may occur due to US tariffs, with some Cabinet Ministers pushing for a delay.
Drinks Ireland said that it provided “much-needed relief” for drinks producers in the country:
In these uncertain times, companies must be as competitive as possible to survive in international markets. This means tackling regulatory burden and reducing costs for producers.
The introduction of supplementary requirements uniquely for the Irish market would have placed additional pressure on all companies operating here, and this would of course be more pronounced for SMEs.
In Business Plus, the Irish Whiskey Association also welcomed the decision, stating that:
The proposed labelling legislation would have significantly increased packaging and labelling costs for our members, in some cases by over 35%.
Alcohol Action Ireland (AAI) said it was disappointed and it was a “blow for public health”, with CEO Dr Sheila Gilheany saying:
It’s not just that the government is allowing its own groundbreaking legislation to be undermined by the very industry it is designed to regulate, this delay will have real-life consequences that will be felt by ordinary Irish people every day. Labels are crucial to efforts to reduce incidences of cancer, liver disease, and foetal alcohol spectrum disorder in Ireland and indeed to change the conversation about this product which is heavily marketed as risk-free and essential to everyday living.
The Irish Medical Association agreed with that sentiment, stating that:
It will result in preventable incidences of cancer, increased incidences of liver disease, and harm to children because of a refusal to fully enact a bill signed into law seven years ago.
In the letter of the day in the Irish Times, Dermot O’Rourke writes about losing his daughter earlier this year as a result of alcohol addiction. He says that the contents of Minister for Enterprise Peter Burke’s letter to the Minister for Health, Jennifer Carroll MacNeill, asking her to consider pushing back on the health warning labels on alcohol products, are shocking. Similarly, AAI described the Irish Government’s alcohol policy as “disjointed and often contradictory” and criticised some cabinet ministers for putting “extreme pressure” on the health minister to scrap or delay health warning labels.
In the build-up to the decision, Dr Gilheany of AAI also said a decision to delay would be “bizarre, because these labels are already on multiple products in multiple shops right across the country.”

In related news, an independent review of Ireland’s National Drugs Strategy (NDS) criticised the lack of integration of alcohol policy, despite alcohol remaining Ireland’s most harmful drug – consumed by 73% of the population, with 1 in 5 drinkers meeting the criteria for alcohol use disorder.
Welsh Government backs minimum unit pricing but signals review of price level ahead of public consultation
The Welsh Government published a report on the operation and effect of the minimum pricing provisions, based on evidence collected in a recent consultation. In a Cabinet statement, the government explained that the introduction of MUP coincided with the start of the pandemic and was followed by the cost of living crisis, which both introduced “significant complexity to the evaluation process”. However, they explain that independent evaluations have concluded that the policy has led to generally positive findings.
The government therefore considers MUP as contributing “towards its intended policy objectives”, but that any future considerations need to take into account the level at which MUP is set. They have commissioned the Sheffield Addictions Research Group to examine this issue. These results will help inform a government proposal on the future of MUP, which will be subject to a public consultation.
The statement concludes that MUP is one of a range of policies and isn’t designed to work in isolation, and the government will continue its work on prevention, support and recovery, and tackling availability.
Parliament debates link between alcohol and cancer for first time
In a landmark Westminster Hall debate on 08 July 2025, MPs gathered to discuss the link between alcohol and cancer – marking the first time the UK Parliament has dedicated a debate solely to the subject, nearly 40 years after alcohol was classified as a Group 1 carcinogen alongside tobacco and asbestos.
Opening the debate, Labour MP Cat Smith expressed disbelief that such a conversation had taken so long:
I find it astounding that although alcohol has been designated a group 1 carcinogen since 1988… almost 40 years later, this is the first debate in this place on alcohol and cancer.

MPs highlighted the scale of alcohol’s role in cancer risk. Alcohol is linked to around 17,000 cancer cases in the UK each year. Breast cancer is the most common cancer associated with alcohol, with one in 10 cases attributed to drinking. Public health modelling suggests that if drinking levels remain high in the wake of the pandemic, the UK could see an additional 18,875 cancer cases by 2035.
A major concern raised during the debate was the stark inequality in outcomes. Rates of alcohol-related cancers and deaths are disproportionately high in the most deprived communities, despite people there often drinking less on average than wealthier groups. Awareness is also low, with a new World Cancer Research Fund poll finding that just 7% of UK adults are aware of the link between alcohol and cancer, and a quarter believe drinking poses no health risk at all.
Several MPs pointed to the wider societal cost of alcohol harm. In England alone, alcohol costs the economy an estimated £27 billion annually – more than double the revenue it generates through taxation.
Frank McNally MP called for early intervention, saying:
This debate is especially pertinent, as we now understand that at least eight cancers can be linked to alcohol… I would like to focus on the importance of early intervention in tackling excessive alcohol consumption.
In response, Public Health Minister Ashley Dalton acknowledged that alcohol is indeed a group 1 carcinogen and agreed that alcohol deaths and wider harm are unacceptably high, pointing to 103,000 hospital admissions due to alcohol-related cancers last year alone. She highlighted the government’s ongoing investment in local alcohol treatment services and the rollout of new alcohol treatment guidelines. Pilot liver health screening programmes have reached nearly 125,000 people in primary care, identifying thousands with liver damage and enrolling over 9,000 into liver cancer surveillance pathways. Dalton also acknowledged that liver cancer rates have risen by 50% in the last decade, driven in large part by alcohol-related liver disease.
MPs from across parties called for greater public awareness campaigns, mandatory health labelling on alcohol products, and a stronger focus on prevention through early diagnosis and harm reduction.
While no policy commitments were made during the debate, it signalled a growing recognition that alcohol’s role in cancer cannot be ignored. As Smith concluded, this debate could be a turning point in shifting alcohol from a matter of individual lifestyle to a serious and under-recognised public health risk.
In a follow up article in Parliament News, Smith called for better public education, mandatory labelling, stricter regulation of marketing, and a comprehensive national alcohol strategy.
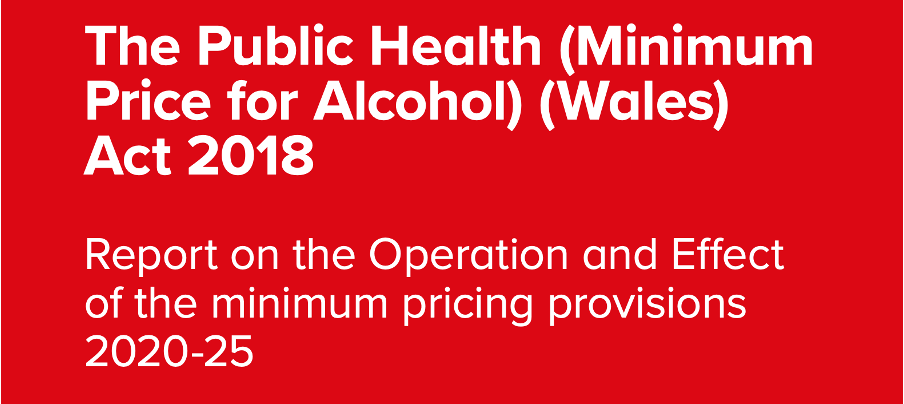
Alcohol duty reforms target heavy drinkers and wealthier people
A new study published in the Journal of Public Health found that the UK’s 2023 alcohol duty reform is likely to increase spending for the heaviest drinking households – while having little or no impact on lighter drinkers.
The research, led by Dr Luke B. Wilson from the University of Sheffield, analysed household alcohol purchases. The policy, implemented in August 2023, replaced a mixed taxation system with one based solely on alcohol strength and was brought in alongside a 10.1% duty rate increase in response to inflation.
The study found that the structural reform alone would increase average household alcohol spending by just 0.59%. However, this rise is concentrated in the top 20% of alcohol-purchasing households, while spending for the remaining 80% is expected to fall.
Relative impacts of duty reform scenarios on household spending on alcohol by purchaser quintile
Our results provide some support for the structural reforms to alcohol duty being effectively targeted at the heaviest alcohol purchasers, with no evidence to suggest that they are likely to increase economic inequalities – said Wilson in a blog for IAS.
However, this targeting effect was weakened somewhat by the inclusion of the ‘wine easement’, a temporary measure introduced following industry lobbying.
When the duty rate increase is included, the average rise in household alcohol spending jumps to 5.37%, with the largest impacts again among the heaviest purchasers. Households in higher socioeconomic groups also face slightly higher increases, largely due to purchasing more alcohol.
While the reforms may support public health goals, the study concludes they are unlikely to offset the impact of real-terms duty cuts over the past decade or significantly reduce alcohol-related harm on their own.
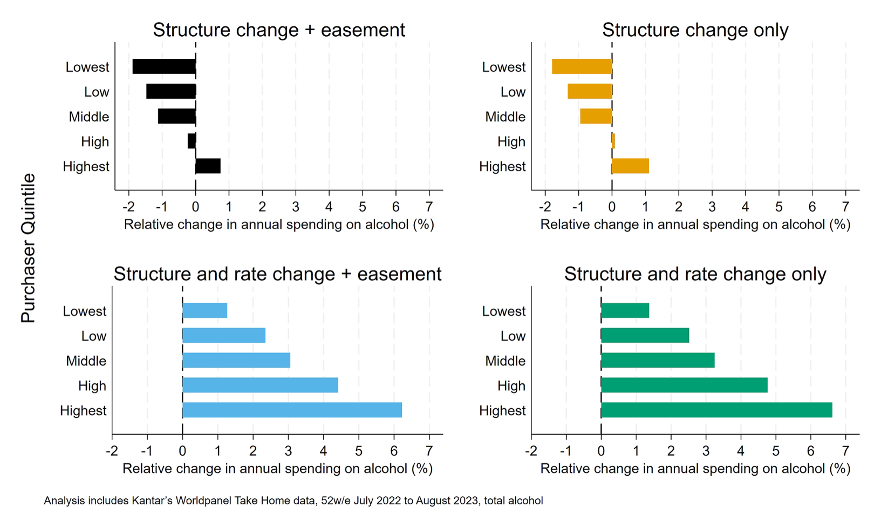
1 million at risk of ‘triple threat’ of smoking, drinking, and overweight
1 million people in England are living with the triple threat of being overweight, drinking over the guidelines, and smoking, research from Action on Smoking and Health (ASH) has found (and reported in The Guardian).
This means that their risk of diseases such as cancer and diabetes is significantly higher and increases their risk of dying much earlier than the average person.
The analysis also found that 10 million have two of the three risky behaviours, while 34 million have at least one.
Professor Sir Ian Gilmore said:
When these risk factors are combined, the danger to people’s health is even greater, leading to higher chances of early death and more years in poor health. Together they create a toxic combination that can lead to long-term disability and early death.
Although the risks of two or more risk factors are not purely additive, it is likely that smoking, grade three obesity and heavy drinking will reduce life expectancy by at least 20 years.
Caroline Cerny, the deputy chief executive of ASH, said:
The findings are extremely worrying. They provide an insight into the challenges facing the NHS both now and in the future.
Drugs, Alcohol & Justice APPG calls for a national alcohol strategy

The Drugs, Alcohol & Justice APPG has launched its Action on Alcohol Harm report in Parliament – supported by Via, Waythrough, and With You – which warns that the UK is facing a deepening alcohol crisis, with record levels of harm and inadequate support services.
The report calls for long-term investment in alcohol treatment and recovery services, with a national, cross-government strategy to coordinate efforts and reduce inequalities.
Key recommendations include expanding community-based support, embedding lived experience organisations, improving access to treatment in prisons, and prioritising preventative public health policies such as MUP and better labelling.
The report also urges greater use of diversion schemes and community sentences for alcohol-related offences, rather than punishment alone.
Chair of the APPG, Grahame Morris MP, said:
We know what works. With the right political leadership, we can turn the tide on alcohol harm.
WHO launches initiative to raise health taxes and save millions of lives
The World Health Organization (WHO) has launched a new project called the “3 by 35” initiative, urging countries to raise real prices on tobacco, alcohol, and sugary drinks by at least 50% by 2035.
It aims to reduce chronic diseases and raise public revenue.
The consumption of tobacco, alcohol, and sugary drinks are fuelling the NCD epidemic. NCDs, including heart disease, cancer, and diabetes, account for over 75% of all deaths worldwide. A recent report shows that a one-time 50% price increase on these products could prevent 50 million premature deaths over the next 50 years.
The initiative has an ambitious but achievable goal of raising US$1 trillion over the next 10 years. Between 2012 and 2022, nearly 140 countries raised tobacco taxes, which resulted in an increase of real prices by over 50% on average, showing that large-scale change is possible.
Alcohol Toolkit Study: update
The monthly data collected is from English households and began in March 2014. Each month involves a new representative sample of approximately 1,700 adults aged 16 and over.
See more data on the project website here.
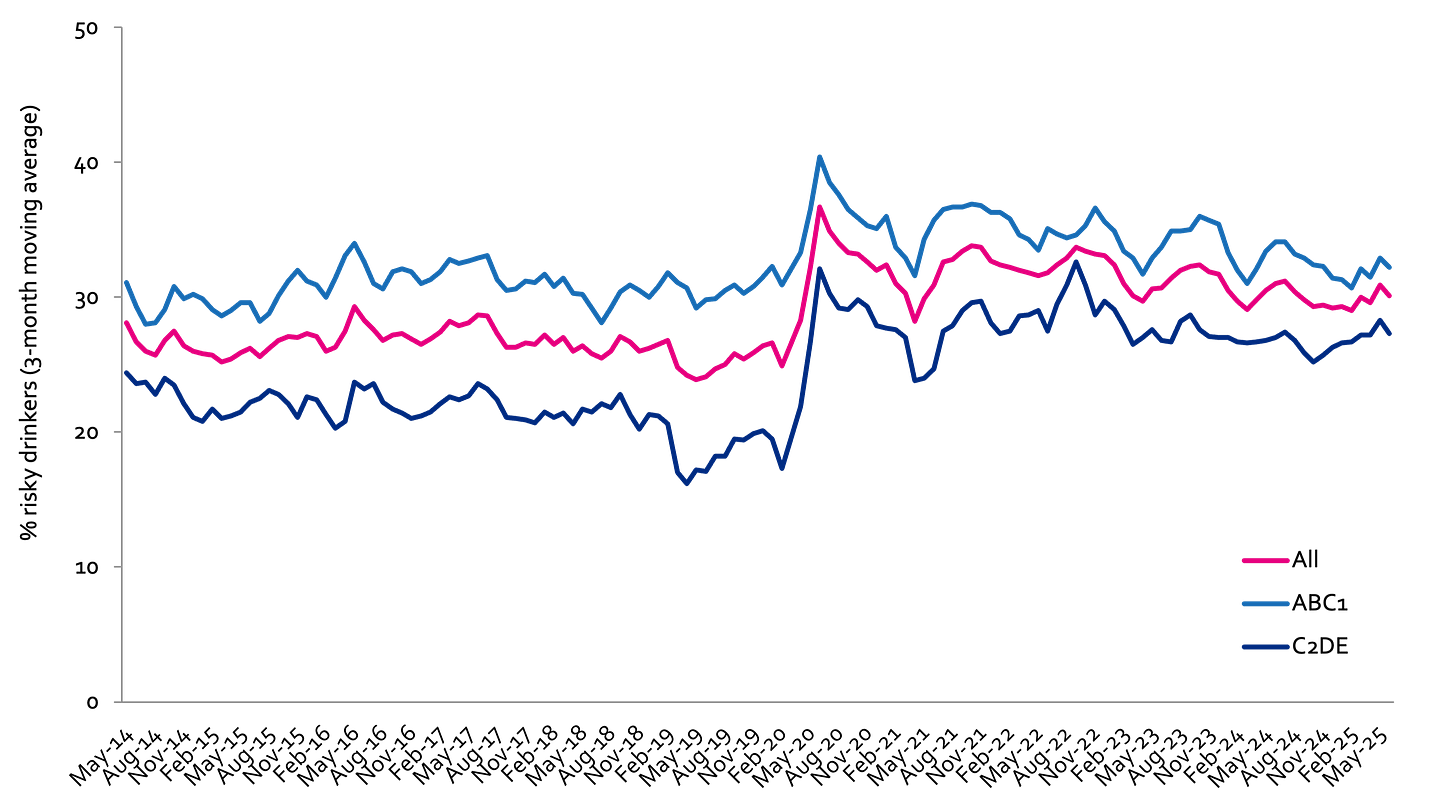
Prevalence of increasing and higher risk drinking (AUDIT-C)
Increasing and higher risk drinking defined as those scoring >4 AUDIT-C. A-C1: Professional to clerical occupation C2-E: Manual occupation
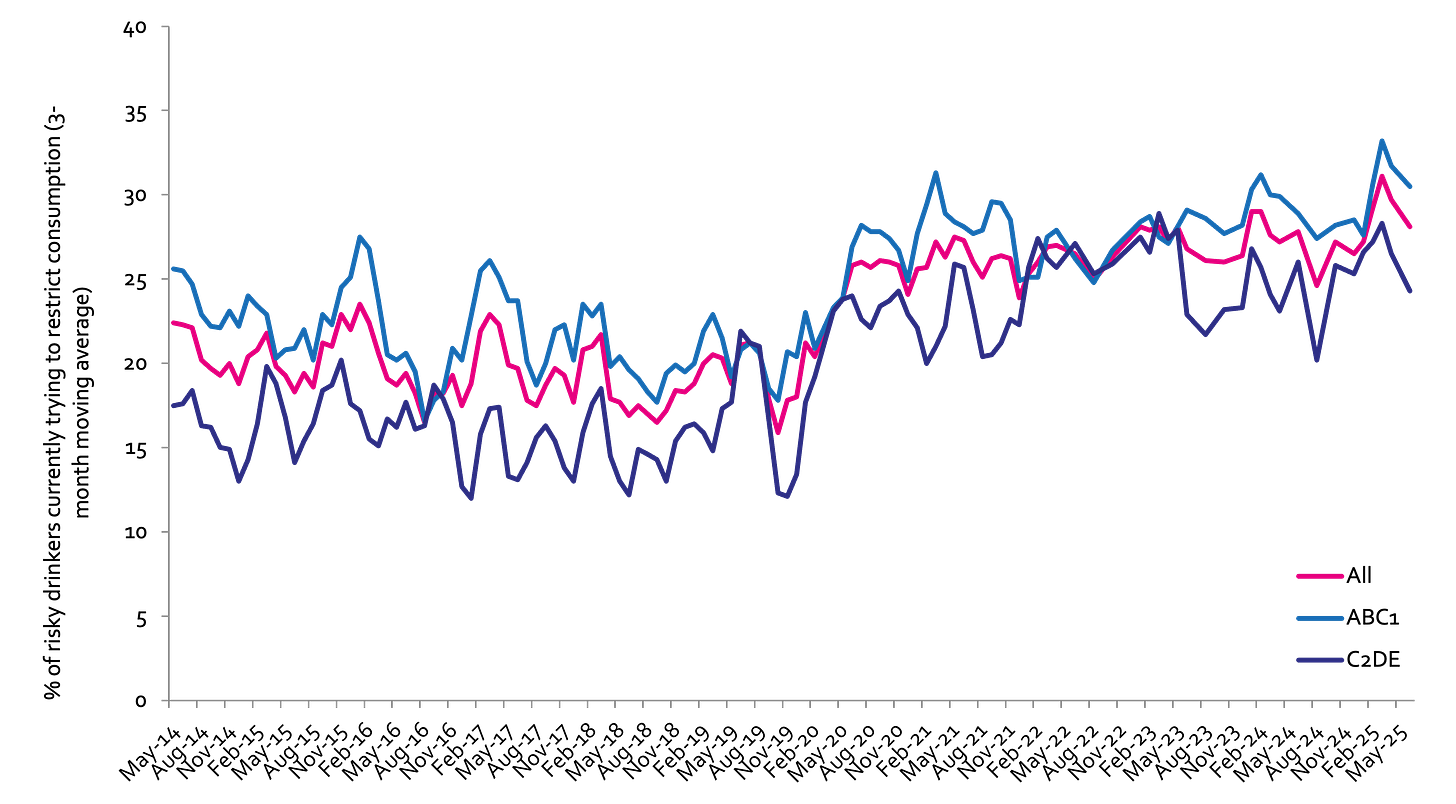
Currently trying to restrict consumption
A-C1: Professional to clerical occupation C2-E: Manual occupation; Question: Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses? Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses?
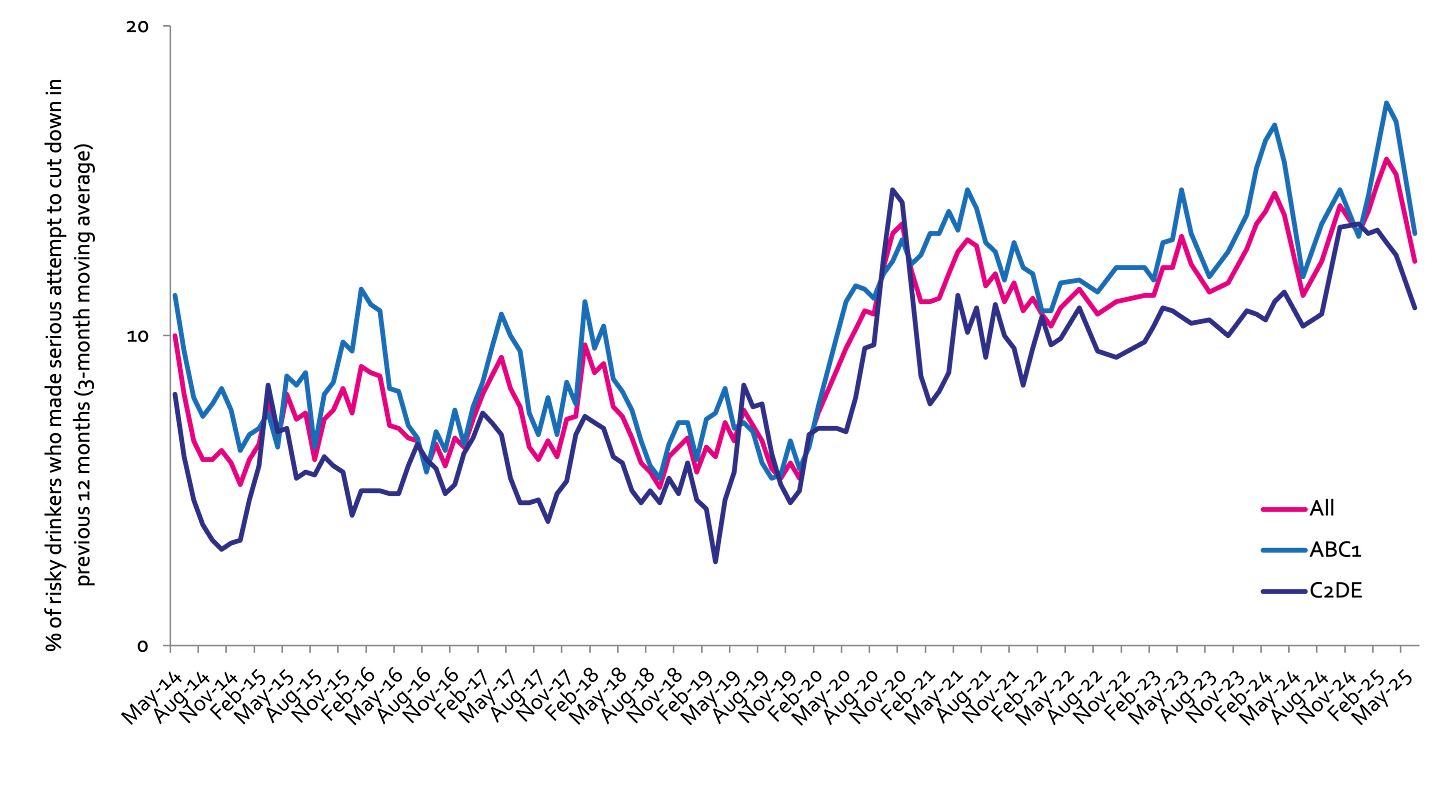
Serious past-year attempts to cut down or stop
Question 1: How many attempts to restrict your alcohol consumption have you made in the last 12 months (e.g. by drinking less, choosing lower strength alcohol or using smaller glasses)? Please include all attempts you have made in the last 12 months, whether or not they were successful, AND any attempt that you are currently making. Q2: During your most recent attempt to restrict your alcohol consumption, was it a serious attempt to cut down on your drinking permanently? A-C1: Professional to clerical occupation C2-E: Manual occupation
Podcast
Our monthly podcast features interviews with experts from across the sector.
Plans to reduce drink-drive limit in England and Wales
Luca Straker –
Brake - the road safety charity