In this month’s alert
Developing a roadmap for tackling alcohol harm in the UK – podcast feature
On this month’s podcast we spoke to Dr Katherine Severi, IAS’s Chief Executive, and Karen Biggs, Chief Executive of treatment provider Phoenix Futures, about IAS’s forthcoming report: A healthier future: A long-term vision to tackle alcohol harm in the UK, due to be published in October.
We discussed why a long-term strategy is urgently needed, the ambitious targets set out in the report, and how prevention and treatment must go hand in hand. The conversation explored both the opportunities and barriers ahead – from minimum unit pricing and stronger marketing restrictions, to the postcode lottery in treatment and the influence of the alcohol industry.
As Dr Katherine Severi puts it:
There’s no magic pill or silver bullet. That’s why our report sets out a broad range of policies and clear targets – not only to build capacity in treatment and support services, but also to ‘turn down the tap’ and prevent the next generation from experiencing alcohol harm.
Alcohol-specific deaths in Scotland fall by 7%
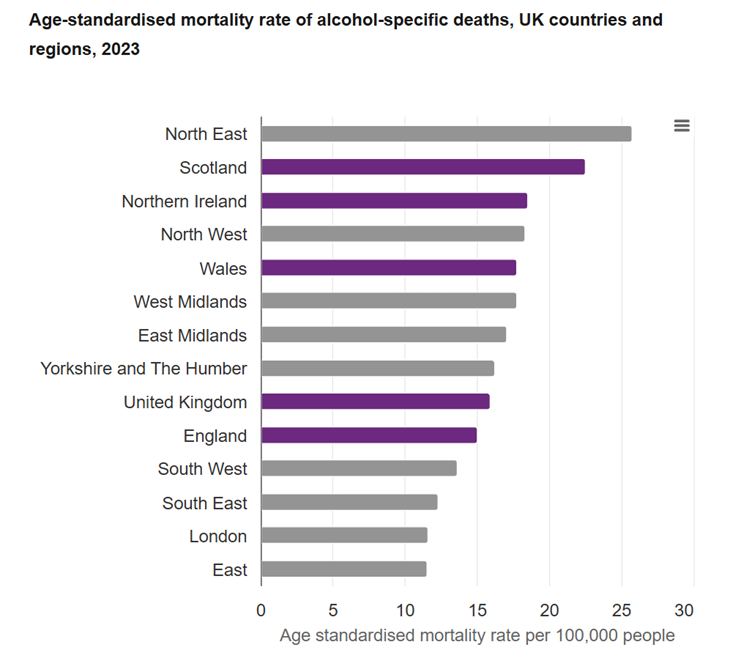
Recent figures from the National Records of Scotland reveal a step forward in tackling alcohol-related harm, as the number of alcohol-specific deaths in Scotland dropped by 7% in 2024.
In total, 1,185 alcohol-specific deaths were registered, 92 fewer than in 2023, and the lowest annual figure since 2019. When accounting for age, the alcohol-specific mortality rate decreased to 20.9 deaths per 100,000 people, down from 22.5 the previous year. Men continued to represent about two thirds of these deaths, but decreases were observed in both male and female categories over the past year.
However, the data also highlight ongoing health inequalities: people living in the most deprived areas experience a death rate from all causes twice as high as those in the least deprived, and for alcohol-specific causes, the rate is 4.5 times higher.
Dr Peter Rice, chair of the Institute of Alcohol Studies, said:
Compared to the rest of the UK, Scotland had made real progress in reducing alcohol deaths over the past 20 years. From a starting point of a substantial gap, Scotland’s alcohol death rate is now close to, and at times below, the northern regions of England and Northern Ireland.
The Scottish experience shows that harm from alcohol can be reduced by a well-planned alcohol strategy, but actions must be sustained and developed.
Public opinion polling reveals what voters think about public health
The quality of the NHS is the second most important issue facing the country, according to a survey of 2,010 adults conducted by Public First, ranking behind only the cost of living, and ahead of issues like immigration and the state of the economy. Most respondents also link today’s NHS pressures to the widespread use of products that harm health, including alcohol, unhealthy food and drink, and tobacco.
People want government to do more than just treat illness, with action on the root causes of poor health, but how do Conservative, Labour and Reform voters differ on how they view public health?
Analysis by Action on Smoking and Health (ASH) found that party labels mattered less than expected. While supporters of different parties start from different instincts, backing for practical health measures frequently crosses the usual ideological divides.
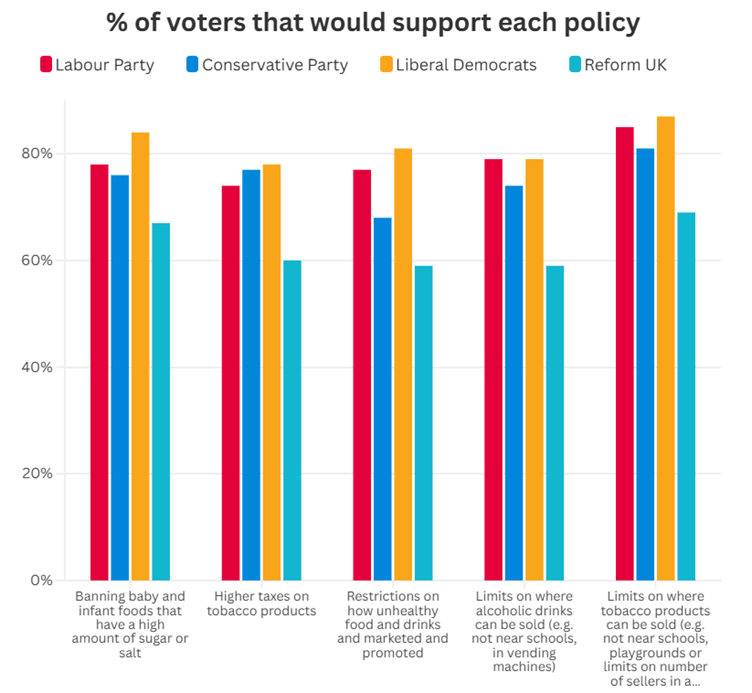
ASH have produced a series of briefings covering quantitative and qualitative data on what different sets of voters think about public health policies, and implications and insights about how to discuss health with voters and politicians of different political leanings.
New Chief Medical Officer report on health trends in England
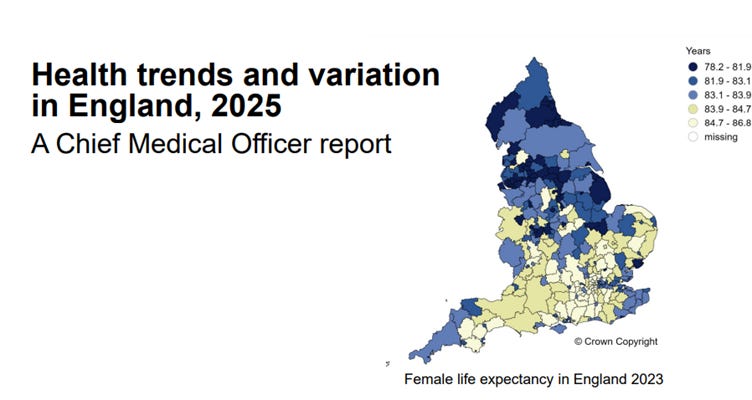
The Chief Medical Officer’s annual report (CMO) provides a snapshot on health in England, showing major trends over time and highlighting the very substantial variation in good and poor health over geography, socioeconomic status, gender, age and ethnicity.
The latest report has revealed a complex picture of alcohol consumption and its impact on public health. Alcohol has become increasingly more affordable: since 2000, the average price per unit of alcohol has increased in the on-trade more than the off-trade; the volume of alcohol sold per adult increased in the off-trade and decreased in the on-trade sector.
Abstaining from alcohol is more common today than in the mid-1990s, with larger changes in younger age groups. Indeed, the proportion of 15-year-olds who report drinking alcohol in the last week has continued to decline.
In 1996, high risk drinking was more prevalent among young adults, whereas in 2022, it was more common among older adults. The CMO reports that it is likely this cohort effect will be sustained.
Death rates from alcohol have increased, particular among males, who are more likely to drink at levels that increase risk of harm compared with females. Despite the proportion of adults who reported drinking at risky levels being similar across deprivation levels, the rate of deaths related to alcohol remains greater in more deprived areas.
CMO Professor Sir Chris Whitty’s report emphasises how some communities and geographies have been left behind, suffering very high burdens of largely preventable disease: “Addressing these disparities and inequalities has to be a major priority of public health and the NHS.”
Independent review finds alcohol marketing to be pervasive and persuasive
Public Health Scotland (PHS) was tasked by the Scottish Government to provide evidence that could inform ministers about possible strategies for regulating alcohol marketing.
Their rapid review demonstrated compelling evidence that alcohol marketing significantly increases consumption and contributes to alcohol-related harm, particularly among children and young people. Alcohol advertising is extremely prevalent—in sports, on public transport, in shops, and online—and being exposed to such marketing is associated with stronger intentions to drink, higher levels of consumption, and riskier drinking behaviours. The report emphasised that contrary to claims from the alcohol industry, marketing does not merely influence brand preference but leads to higher overall consumption, attracts new drinkers, and specifically targets heavy drinkers.
Voluntary self-regulation by the industry has proven ineffective. In contrast, regulations that restrict alcohol marketing, especially when implemented comprehensively rather than partially, can reduce exposure, consumption, and associated harms. Given Scotland’s high rates of alcohol-related harm, these findings present a robust case for the Scottish Government to adopt stronger measures limiting alcohol marketing, in keeping with recommendations from the World Health Organization.
Alison Douglas, chief executive of Alcohol Focus Scotland, said:
Children and young people have the right to a childhood free from alcohol marketing. The Scottish Government has stated time and again that they remain committed to protecting children and young people from alcohol marketing, but they are way behind the curve when it comes to action when compared to other European countries including Ireland. We have the evidence; it’s time to act.
Dr Alastair MacGilchrist OBE, Chair of Scottish Health Action on Alcohol Problems, echoed these concerns:
The review concludes that voluntary self-regulation by the industry is not working. The evidence supports a complete ban; however it is reasonable to assume that since more marketing results in higher sales and consumption, any reduction in marketing will lead to lower sales and therefore less harm.
Experts urge the Government to deliver on prevention
Chief executives from the Health Foundation and the King’s Fund have together called for the Government to accelerate action on prevention or risk further decline in public health.
The UK is experiencing rising rates of chronic illness, stalling life expectancy, and widening health inequalities. Poor workforce health is costing employers up to £150 billion annually in lost productivity, while the UK’s mortality rates are worsening compared to other wealthy countries. The impact is felt across society, with millions facing diminished quality of life and the government forced to choose between rising healthcare costs or accepting poorer care and deeper inequalities.
Despite ambitious promises of a ‘prevention revolution’ to address the root causes of poor health, recent government strategies have focused narrowly on the NHS rather than broader determinants of health, and the mission delivery unit has been scrapped, raising concerns about lasting commitment.
While some positive steps have been taken, including tobacco and vapes legislation and improved mental health support, key measures like minimum unit pricing for alcohol remain absent. Sarah Woolnough (King’s Fund) and Jennifer Dixon (Health Foundation) described how industry lobbying from food and alcohol firms continues to weaken and delay evidence-based policies, with vested interests opposing interventions that would improve public health.
To make tangible progress, they recommend the following:
- Bold interventions to tackle these unhealthy behaviours e.g., raising alcohol taxes, restricting junk food advertising, and tackling inequalities.
- Commission a rapid audit on the health of the nation and what should be done.
- Reboot the health mission with a cross-government 10-year plan for rebuilding the health of the nation.
- Ensure genuine accountability with independent reporting on progress and future trends.
- Tackle fiscal rules that deter investment in prevention
- Invest in local public health services, returning the public health grant to a real-terms equivalent of 2015/16 per person.
Without urgent and courageous leadership, the NHS risks collapsing under preventable illnesses, and the country’s health and economy will continue to suffer.
Alcohol industry lobbying and Irish labelling delays
Ireland was set to become one of the first countries in the world to introduce comprehensive alcohol labelling under section 12 of the Public Health (Alcohol) Act. The policy was signed into law in May 2023, giving producers a three-year lead-in time to planned implementation in May 2026. However, the introduction of this much-needed measure experienced a further setback recently when the Government announced a delay in its implementation until 2028.
Industry lobbying has been identified as a key factor in delaying public health measures like these. One study analysed 16 submissions from alcohol industry actors to the European Commission regarding Ireland’s proposed alcohol warning label regulations. Thematic analysis revealed that these submissions repeated four main themes: lack of evidence supporting the content of health warning labels and their broader use, negative trade and economic impacts of mandatory health warning labels, potential risks to EU governance posed by Ireland’s labels, and the industry’s self-positioning as responsible actors committed to public health.
The analysis suggests that industry actors strategically adapt their arguments to varying institutional settings and policy instruments, demonstrating their political dexterity and reinforcing the barriers to policy progress.
New studies reveal rise in alcohol-free drink consumption but question public health impact
The recent 10 Year Health Plan for England included ambitions to reduce alcohol harm by supporting growth in the no- and low-alcohol market.
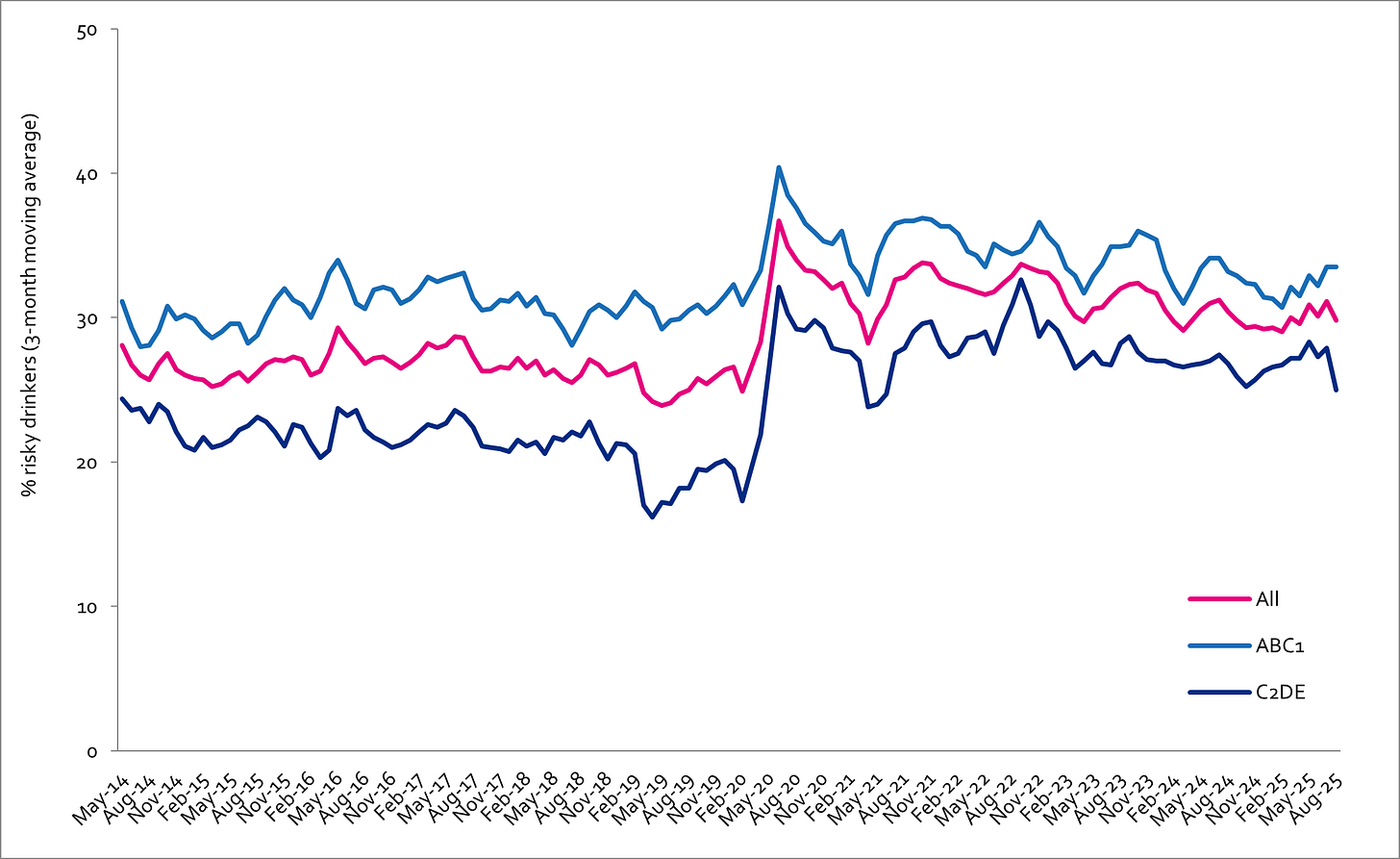
Studies from the University of Sheffield and University College London have shed fresh light on the growing popularity of alcohol-free and low-alcohol drinks among British adults, particularly those consuming alcohol at risky levels.
Researchers from the University of Sheffield found that found that one in three adults in the past year have tried an alcohol-free or low-alcohol drink. Those identified as “risky” drinkers were more likely to purchase these alternatives regularly. However, analysis of household shopping habits indicated that 96% of households buying “no/lo” beverages also bought alcoholic drinks, suggesting that these products are being used alongside, rather than as a substitute for, alcohol.
Pricing disparities may undermine the potential health benefits. While alcohol-free wines, spirits, and ready-to-drink beverages were generally cheaper than their alcoholic counterparts, alcohol-free beers and ciders were found to be more expensive. Professor John Holmes, director of the Sheffield Addictions Research Group, warned that such affordability barriers could limit the benefits for more deprived groups, who are most at risk of alcohol-related harm.
In parallel, researchers at University College London published a study analysing data from the Smoking and Alcohol Toolkit Study. Among nearly 9,400 adults identified as higher-risk drinkers who had tried to cut down, the use of low and no-alcohol drinks as a reduction strategy increased from 35% to 44% in serious attempts between October 2020 and August 2024. The most notable rise occurred among older adults, who initially reported less use. However, the use of evidence-based support for cutting down—either alone or combined with no/low-alcohol options—remained consistently low.
Researchers called for urgent further research to determine the true effectiveness of alcohol-free and low-alcohol drinks in reducing consumption, and for policy-makers to consider these findings in shaping future public health strategies. While the trend towards “no/lo” alcohol options is clear, experts caution that without wider access and affordability—especially among those most at risk—their full potential to improve public health may not be realised.
Alcohol Toolkit Study: update
The monthly data collected is from English households and began in March 2014. Each month involves a new representative sample of approximately 1,700 adults aged 16 and over.
See more data on the project website here.
Prevalence of increasing and higher risk drinking (AUDIT-C)
Increasing and higher risk drinking defined as those scoring >4 AUDIT-C. A-C1: Professional to clerical occupation C2-E: Manual occupation
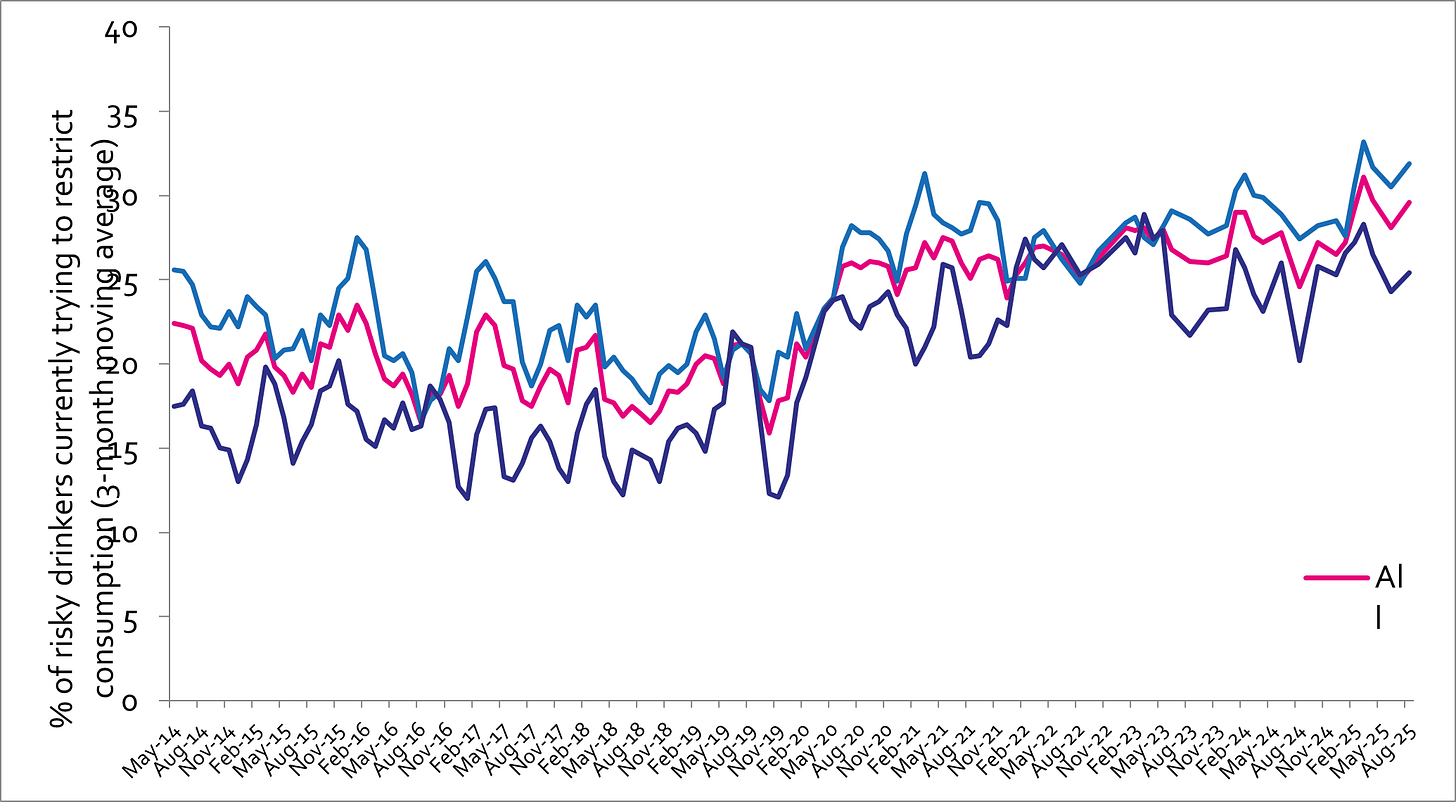
Currently trying to restrict consumption
A-C1: Professional to clerical occupation C2-E: Manual occupation; Question: Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses? Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses?
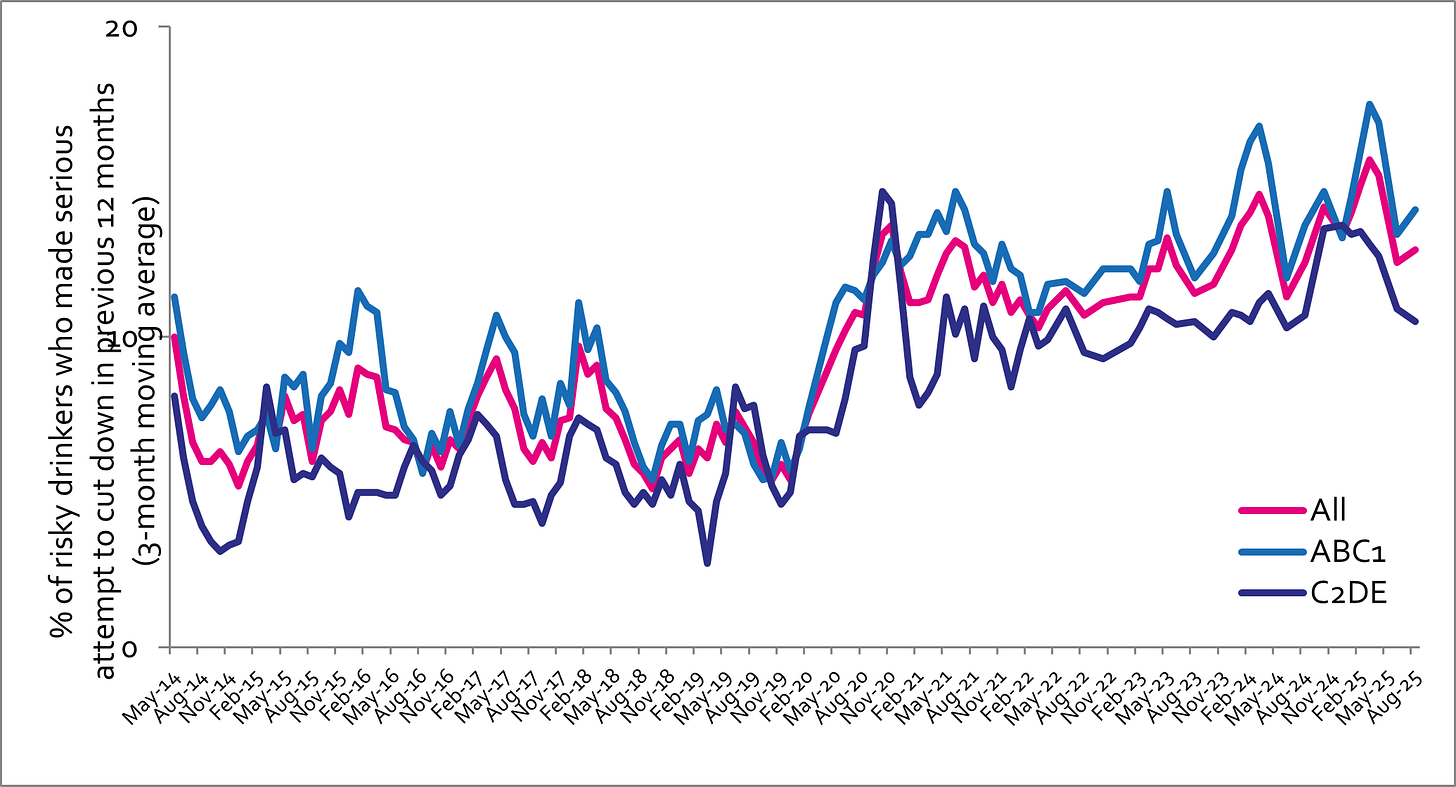
Serious past-year attempts to cut down or stop
Question 1: How many attempts to restrict your alcohol consumption have you made in the last 12 months (e.g. by drinking less, choosing lower strength alcohol or using smaller glasses)? Please include all attempts you have made in the last 12 months, whether or not they were successful, AND any attempt that you are currently making. Q2: During your most recent attempt to restrict your alcohol consumption, was it a serious attempt to cut down on your drinking permanently? A-C1: Professional to clerical occupation C2-E: Manual occupation
Podcast
Our monthly podcast features interviews with experts from across the sector.
Plans to reduce drink-drive limit in England and Wales
Luca Straker –
Brake - the road safety charity

