In this month’s alert
A Healthier Future: A long-term vision to tackle alcohol harm in the UK
Alcohol harm is at record levels in the UK, with deaths the highest ever reported and the costs to society exceeding £27 billion each year in England alone. People living in our most deprived communities are paying the heaviest price, with rates of liver disease and alcohol-related deaths far higher than in more affluent areas. Yet, despite the scale of the problem, the UK government has not produced a national alcohol strategy since 2012.
In contrast, the tobacco control community has helped drive consistent progress and policy change by working towards a clear shared vision. That kind of unifying roadmap has been missing in alcohol in recent years, with the last independent national strategy, ‘Health First’ published in 2013. This new report helps fill that gap – bringing together a broad coalition of experts in policy, research, treatment, and lived experience to agree on common goals and a practical path forward.
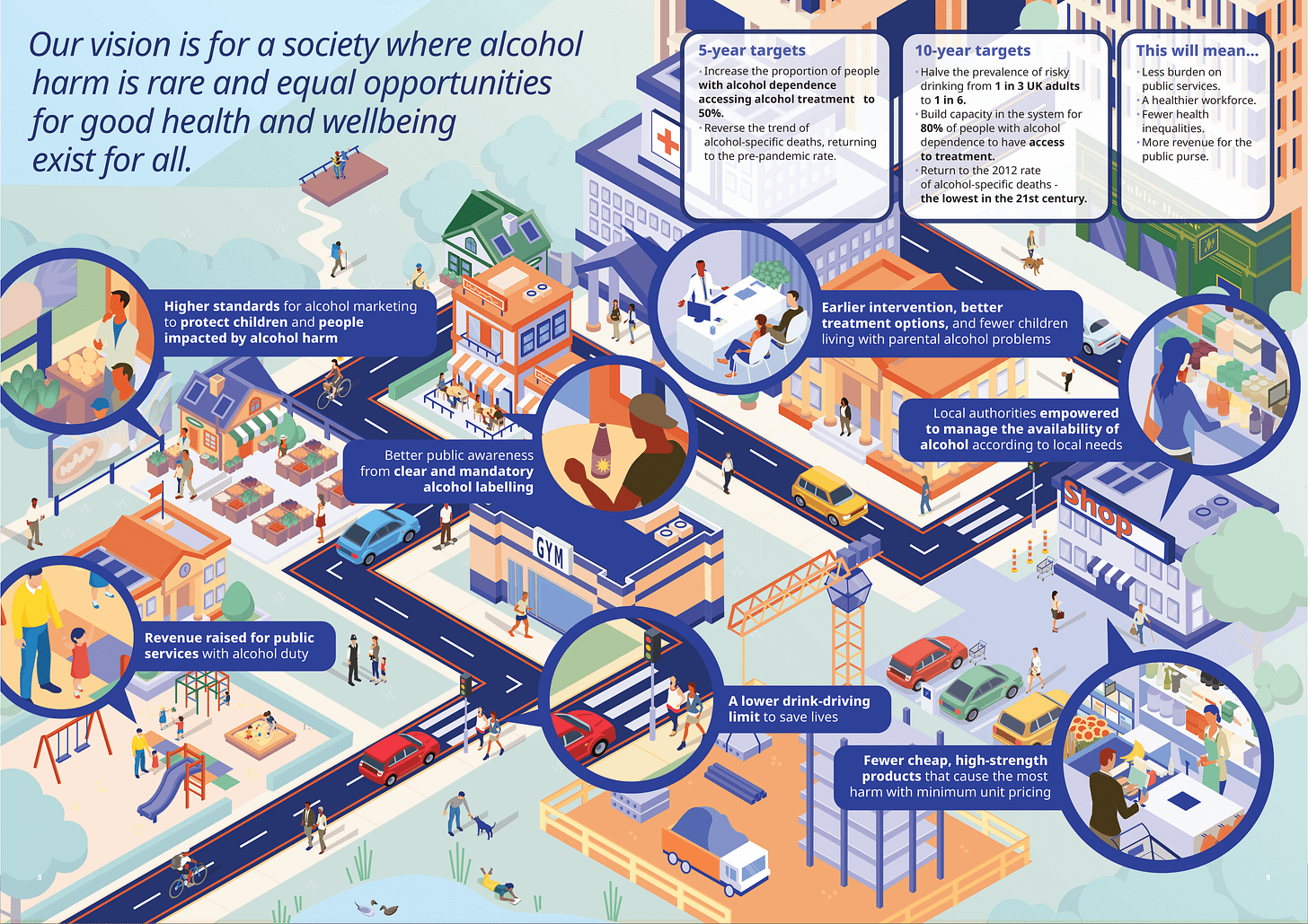
Our vision is for a society where alcohol harm is rare and equal opportunities for good health and wellbeing exist for all.
A Healthier Future: A long-term vision to tackle alcohol harm in the UK sets out ambitious but achievable targets to:

To achieve this, the experts recommend a package of high-impact policies, including:
- Introducing a minimum unit price of 65p in England and uprating it with inflation
- Reinstating the alcohol duty escalator
- Bringing in tougher restrictions on alcohol marketing
- Empowering local authorities to regulate sales and online deliveries
- Sustained investment in treatment and prevention services
- Mandatory health information on alcohol labels
- Lowering the drink-driving limit across the UK
Polling shows strong public support for these measures, with three-quarters of people wanting government to prioritise health over business growth.
Dr Katherine Severi, Chief Executive of the Institute of Alcohol Studies, said:
Alcohol harm is a very broad and complex issue, and there’s no single silver bullet that will solve it overnight. That’s why our report sets out a broad range of evidence-based policies and clear targets – not only to build capacity in treatment and support services, but also to ‘turn down the tap’ and prevent the next generation from experiencing alcohol harm.
The report includes a visual roadmap that lays out the route to achieving these ambitious targets, and can be used in future advocacy work:
We have also developed a short film that explains the purpose of the report and the key targets and policy recommendations.
The report is clear: urgent political leadership is needed to turn the tide on alcohol harm, protect future generations, and build a healthier, fairer society.
Please share the report with relevant colleagues and policymakers.
Alcohol duty will rise in line with inflation
At the Budget yesterday, the Chancellor announced that alcohol duty rates will be increased in line with inflation, therefore staying the same in real terms. The Budget document states:
The government heard representations from stakeholders ranging from a duty cut or freeze to above inflation increases. This decision balances the important contribution of alcohol producers and the hospitality sector to the UK’s culture and economy, with the duty’s role in reducing alcohol harm.
The expectation is the RPI increase will be 3.66% from 01 February 2026, which would increase most beer duty from £21.78 per litre of pure alcohol to £22.58, most wine duty from £29.54 to £30.62, and most spirits duty from £32.79 to £33.99. That would increase nominal duty paid for the following average products:
- A 4% pint of beer from 49p to 51p
- A 12% bottle of wine from £2.66 to £2.76
- And a 40% bottle of vodka from £9.18 to £9.52
The official forecast by the Office for Budget Responsibility explained that:
Alcohol duty receipts are expected to raise £12 billion in 2025-26, a 5.1 per cent decline relative to 2024-25. Receipts are then anticipated to increase to £14 billion by 2030-31, an average rise of 3.4 per cent each year, largely driven by increases to the duty rate that more than offset the impact of lower in-year and forecast consumption.
The quantity of alcohol products sold is forecast to sharply decline by 6.4 per cent this year and remain broadly flat from 2027-28. This is likely driven by a combination of factors such as a growing trend of alcohol moderation, with substitution to no- and low-alcohol alternatives, and a response to higher prices.
Our Chief Executive, Dr Katherine Severi, welcomed the announcement:
We welcome the government’s decision to keep alcohol duty in line with inflation. It sends a clear signal that ministers aren’t bowing to the barrage of misinformation and aggressive lobbying from the alcohol industry. Past cuts to alcohol duty have handed out more than £28 billion in tax breaks to multinational producers, even as alcohol deaths, hospital admissions, and inequality have soared.
This government has chosen the right course today – but to significantly reduce record alcohol deaths and the huge impact it has on our most deprived communities, it really needs a more comprehensive plan. Minimum unit pricing, complemented by a duty escalator, would be the most effective way to bring deaths down. This could be done while supporting pubs by protecting draught duty relief. Since drinking at home is both a huge driver of chronic diseases and damaging to pubs, specifically targeting cheap, supermarket alcohol would be good for public health and pubs.
Tackling alcohol harm is also vital for economic growth, as England alone loses well over £5 billion a year in lost productivity due to alcohol. We desperately need a national alcohol strategy that combines these fiscal measures with other evidence-based policies if we want to see a thriving and healthy population.
Various alcohol industry trade groups criticised the decision, with the CEO of the Wine & Spirit Trade Association saying it was a “typically disappointing and shortsighted decision” that would only prolong a “doom loop” in the economy.
Government licensing reform sparks concerns over public health and local accountability – podcast feature
In our latest podcast we spoke to Professor Niamh Fitzgerald and Dr James Nicholls of the University of Stirling about the UK government’s recent alcohol licensing Taskforce and its proposed reforms. We discussed the implications of the proposals for public health, local accountability, and the hospitality industry, and explored why economic growth arguments are being prioritised over health considerations.
On the episode Dr Nicholls explained that:
This is a pretty unique example of quite fundamental changes being made to the system on the basis of an incredibly short report that was produced in six weeks by a very, very small group of people, most of which was dominated by the alcohol industry themselves.
They highlighted that the six-week Taskforce, dominated by industry representatives, proposed measures including a national licensing policy framework, an “amnesty” on licensing conditions, and enhanced powers for licensing officers. These changes could undermine democratic oversight, weaken local control, and shift the licensing system’s focus from public safety to promoting economic growth.
In related news, Northern Ireland’s Communities Minister, Gordon Lyons, has rejected major reforms to the region’s alcohol licensing system that were recommended by the University of Stirling.

The report argued that existing licensing rules restrict competition and stifle innovation, and it proposed significant changes including replacing the current “surrender principle” with a population-based licensing system overseen by a new licensing authority.
The minister declined to change this system, citing concerns about the financial burden a new authority might place on hospitality businesses already struggling financially.
The decision has been welcomed by some existing licence holders, represented by Hospitality Ulster, who said the proposals created uncertainty for the industry.
However, nightlife campaigners and the report’s authors strongly criticised the move, calling the current system a “closed shop” that benefits private interests and dismisses evidence-based recommendations.
Co-author Dr James Nicholls wrote on LinkedIn that:
Having researched alcohol policymaking for decades, I’m not surprised this kind of thing happens (though this and the recent UK Govt ‘licensing taskforce review’ are quite glaring, from a historical perspective…). It’s also not the first, or even second, time a report into NI licensing has detailed a range of problems and possible reforms, only to be rejected in favour of a uniquely entrenched status quo. It is the role of politicians, not researchers, to make policy decisions – and evidence can (and should) only inform, not determine, policy.
However, only accepting evidence provided by industry – and holding it to no basic standards of accountability or transparency – is a very real problem.
Alcohol consumption is slowly trending towards pre-pandemic levels, but levels of dependence remain high
The prevalence of risky drinking – defined by AUDIT-C scores – appears to be falling back towards levels seen before the coronavirus pandemic, according to a new UCL and University of Sheffield study.
In April 2020, at the start of the pandemic, risky drinking increased by 30.3%, the prevalence of possible alcohol dependence by 90.2%, and mean weekly drinking by 34.5%.
Drawing on data from over 208,000 adults between 2014 and 2024, researchers found that, for most adults, risky drinking levels and mean weekly drinking are slowly trending back toward pre-pandemic levels, though full recovery may take years. In contrast, the prevalence of possible alcohol dependence remains elevated.
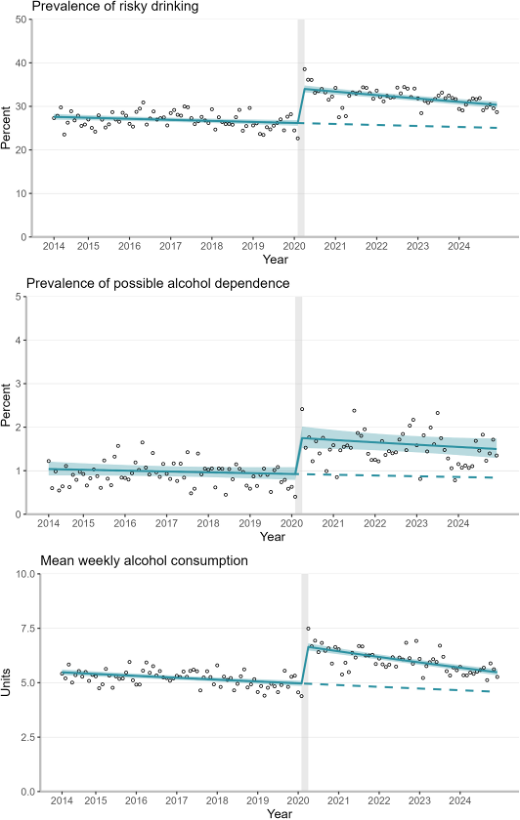
As the authors note:
A further important consideration is that the acute phase of the pandemic was followed by a cost-of-living crisis in the UK, with inflation rising sharply between March 2021 and October 2022. Research has shown that economic crises also impact alcohol consumption, for example, while less disposable income can lead to reduced consumption, increased psychological distress among more vulnerable populations because of a crisis can increase harmful drinking. Despite a decline in overall alcohol sales in the UK since the start of the cost-of-living crisis, it may contribute to sustaining the rise in alcohol-related harm, again, particularly among less advantaged groups who experienced greater increases in psychological distress. Therefore, new alcohol control policies with a focus on narrowing inequalities are required to reduce alcohol-related harm in Great Britain.
Importantly, recovery from these increases varies by social group. Less advantaged drinkers have experienced slower declines in consumption, suggesting that alcohol-related inequalities may be worsening. The findings underline the need for targeted public health policies, including affordability and accessibility measures, to reduce harm and support those at greatest risk.
Barriers to Recovery: Overcoming obstacles to alcohol recovery in the UK
To mark Addiction Awareness Week this week, we have published a new report on Barriers to Recovery, which uses data from interviews with professionals working in alcohol treatment and prevention to describe and discuss the key obstacles currently faced by people with an alcohol dependence across the UK and make recommendations for change.
Key barriers identified include:
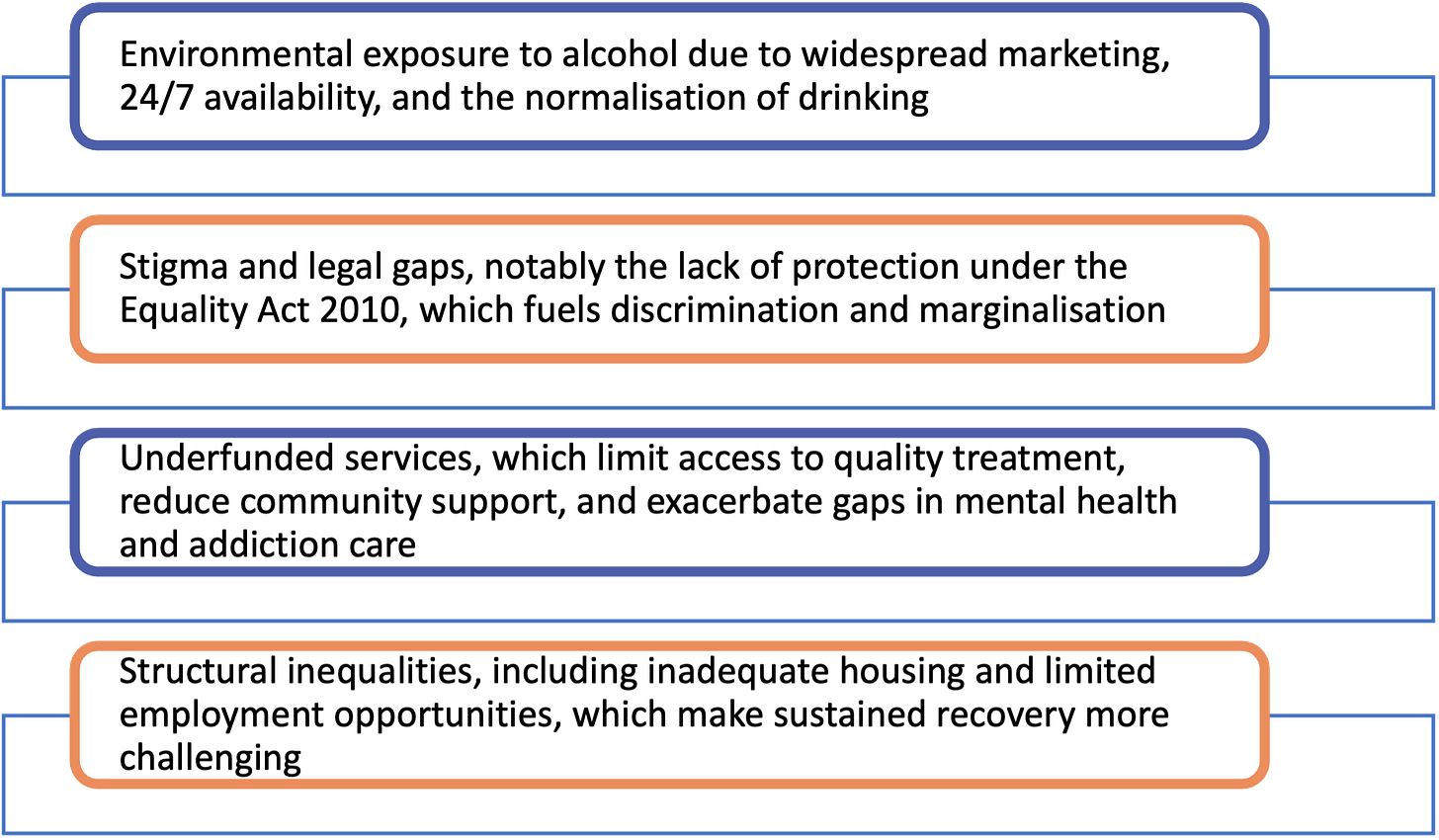
The report makes several recommendations including restricting marketing and availability of alcohol in public spaces, updating the Equality Act 2020 to protect individuals with alcohol dependence, and increasing investment in NHS and community services, housing and reintegration initiatives.
In related news, the Princess of Wales has called for an end to the stigma surrounding addictions, saying the experiences of those dependent on drugs, alcohol or gambling are “shaped by fear, shame and judgment.”
Catherine is patron of the charity Forward Trust. As part of Addiction Awareness Week, which runs up to 30 November, she said:
Addiction is not a choice or a personal failing but a complex mental health condition that should be met with empathy and support.
In an Ipsos survey for the Forward Trust’s Taking Action on Addiction campaign, 53% of 2,124 people questioned said they had personal experience of addiction or knew someone who did.
Eurocare closes Brussels office

Eurocare – the European Alcohol Policy Alliance – has announced that due to funding constraints it will no longer maintain its Brussels office. It will keep its network of over 50 members to ensure coordination on alcohol policy across Europe.
Chair of the Eurocare Board, Dr Peter Rice said:
This is a very difficult time for Eurocare which has been to the forefront of alcohol policy and advocacy at EU level, for over two decades making the public health case to address alcohol harm…While its membership numbers are at an all-time high, unfortunately the scope for accessing EU funding has dramatically reduced.
From January 2026, Eurocare will continue to act as a network of members, sharing information on national and international developments in alcohol policy.
Ambulance staff abused and sexually harassed by intoxicated patients and bystanders

Scottish ambulance staff are frequently being subjected to violence, aggression, and sexual harassment when they attend alcohol-related callouts, according to new research by the University of Stirling.
The first-of-its-kind study – which interviewed ambulance staff about their experiences of intoxicated patients and alcohol-fuelled environments – stated that the repetitive nature of alcohol-related calls led to frustration and reduced morale, and that it diverted paramedics from attending to other patients “whom they see as more legitimately in greater need of emergency medical care”.
Scottish Ambulance Service Chief Executive Michael Dickson told the BBC he was not surprised about the findings, and that they should be used to inform licensing decisions.
Professor Niamh Fitzgerald, the report’s principal investigator, told BBC Scotland News:
It is quite an uncertain environment and it is challenging not just because of the patient’s needs but also the people round about who are also potentially drunk.
The study authors call for greater workplace support, as well as policies to reduce population level alcohol consumption, especially regarding reducing the availability of 24-hour rapid alcohol delivery within the licensing regime.
A Scottish government spokesperson said it was making progress in tackling alcohol harms, with minimum unit pricing saving hundreds of lives and reducing hospital admissions, and recent statistics showing the number of alcohol-specific deaths dropping by 7%.
Professor Sir Ian Gilmore, Chair of the Alcohol Health Alliance, told Emergency Services Times that:
Current UK government plans to make alcohol even more accessible are deeply concerning. They risk exacerbating pressures on ambulance services and making it harder for frontline workers to do their jobs.
Unmasking Influence: How commercial actors influence policy and public health
“Many of the major public health crises we face today are largely driven by powerful corporations. The extent and impact of harmful commercial influences need to be revealed and addressed.”
Dr May van Schalkwyk and Professor Mark Petticrew’s new film Unmasking Influence shares the stories and experiences of those who have dedicated their lives to studying and revealing corporate harm and finding ways to prevent it.
The film focuses on the alcohol, unhealthy food and drink, baby milk formula, pesticides, and tobacco industries, and features experts including Professor Chris van Tulleken, Patti Rundall, Dr Katherine Severi, and Olivier van Beeman.
Alcohol-free drinks: who really benefits?
No- and low-alcohol drinks (NoLos) are growing in popularity, but new evidence shows the picture is more complicated than it seems.
Research from the University of Sheffield finds many NoLo products are more expensive than alcoholic versions – around 5% more for beer in supermarkets and 25% more in pubs, with similar patterns for cider. Zero percent wine was cheaper everywhere, while for spirits prices were lower in supermarkets but higher in pubs.
Industry groups say this reflects production costs, but study author Professor John Holmes warns that if only higher-income drinkers can afford them, “it’s widening the health inequalities already associated with alcohol.”
Professor Holmes et al also published a new commentary in Addiction on the topic, highlighting clinical dilemmas of using NoLo drinks among people with alcohol use disorder. Some may find them helpful for reducing drinking or feeling socially included, while others may face heightened cravings or relapse risk. The authors call for nuanced, patient-centred guidance and better evidence to understand who benefits – and who may be harmed – as the market grows.
Men’s Health Strategy fails to include alcohol control policies

At the end of November, the UK government launched a Men’s Health Strategy to tackle physical and mental health challenges faced by men and boys, and reduce inequalities.
The strategy will focus on suicide prevention, including a partnership on the Premier League’s Together Against Suicide initiative with Samaritans, improved prostate cancer care, targeted treatment for former miners with respiratory diseases, drug and alcohol use, social isolation, and stigma.
Despite wide recognition in the strategy of alcohol’s disproportionate harm to men, there is no mention of the most effective alcohol harm prevention policies. The only policy commits to a £200,000 trial of new brief interventions “to target the rise in cocaine and alcohol-related CVD deaths, particularly among older men” – the pilots will run in acute hospital alcohol care teams.
Professor Gilmore responded to the strategy:
Unfortunately, the Strategy released today falls far short of addressing the key drivers of alcohol harm impacting men.
A comprehensive national alcohol strategy that addresses these issues head-on is urgently needed if we are to reduce inequalities, save lives and support men to live longer, healthier lives.
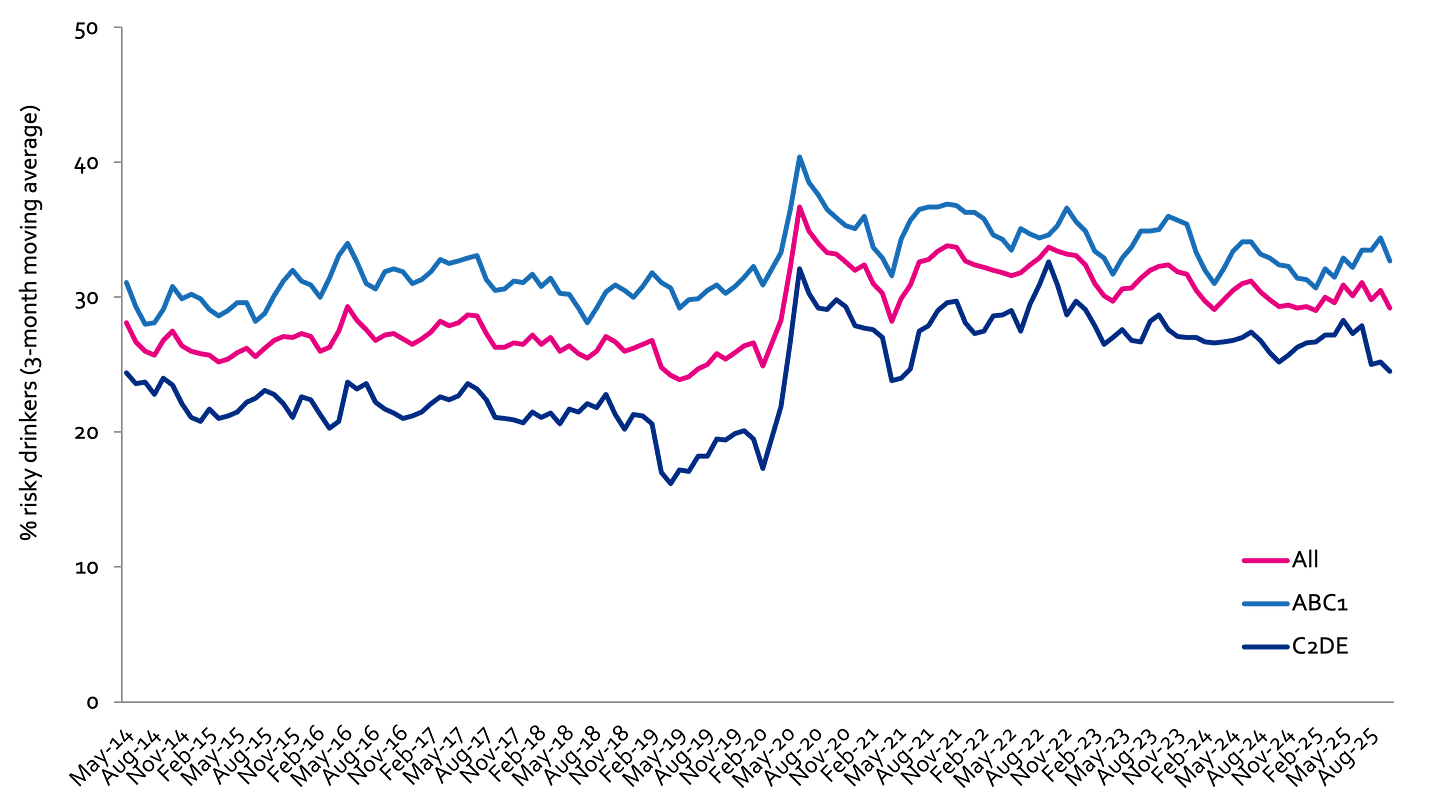
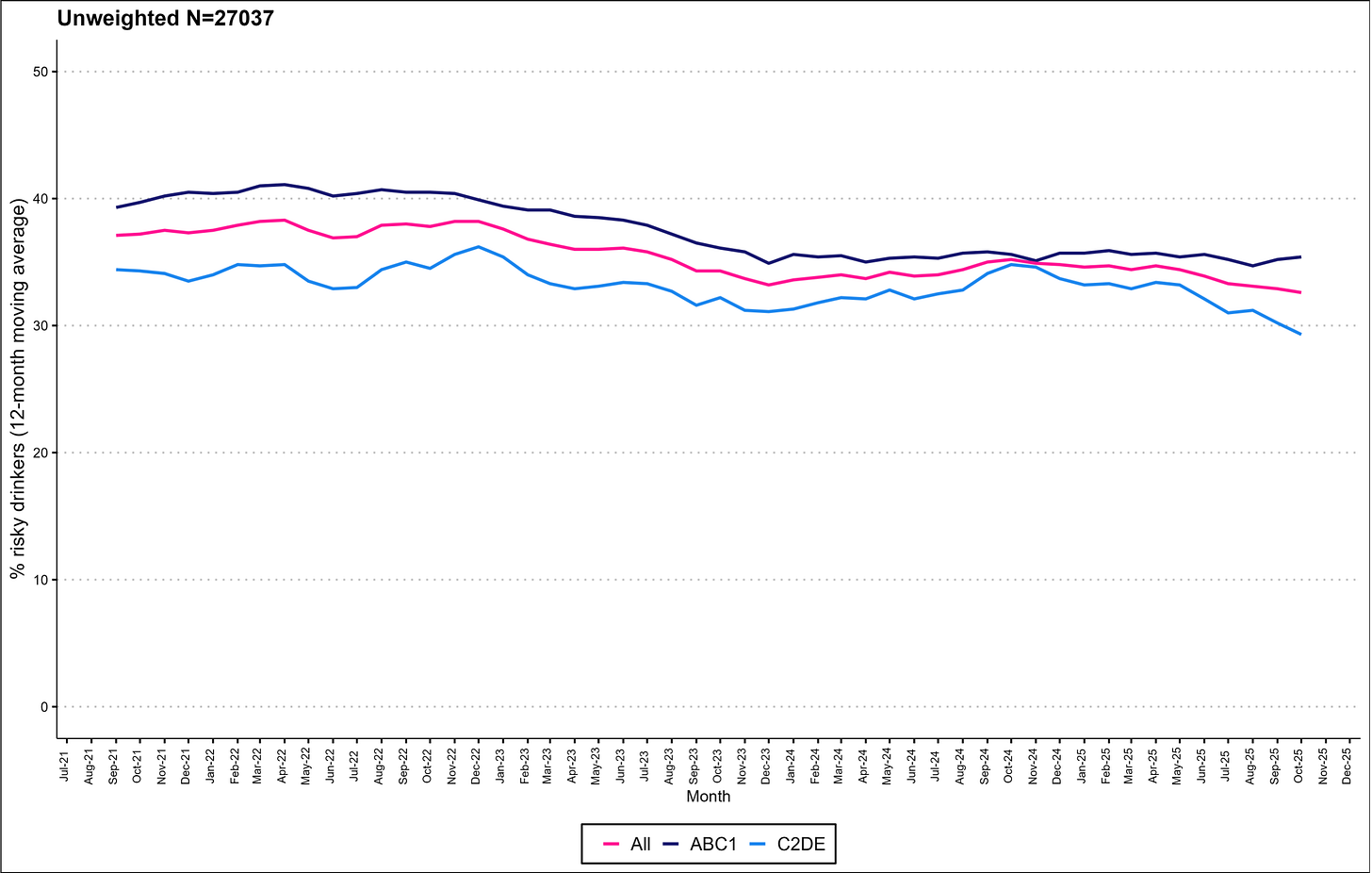
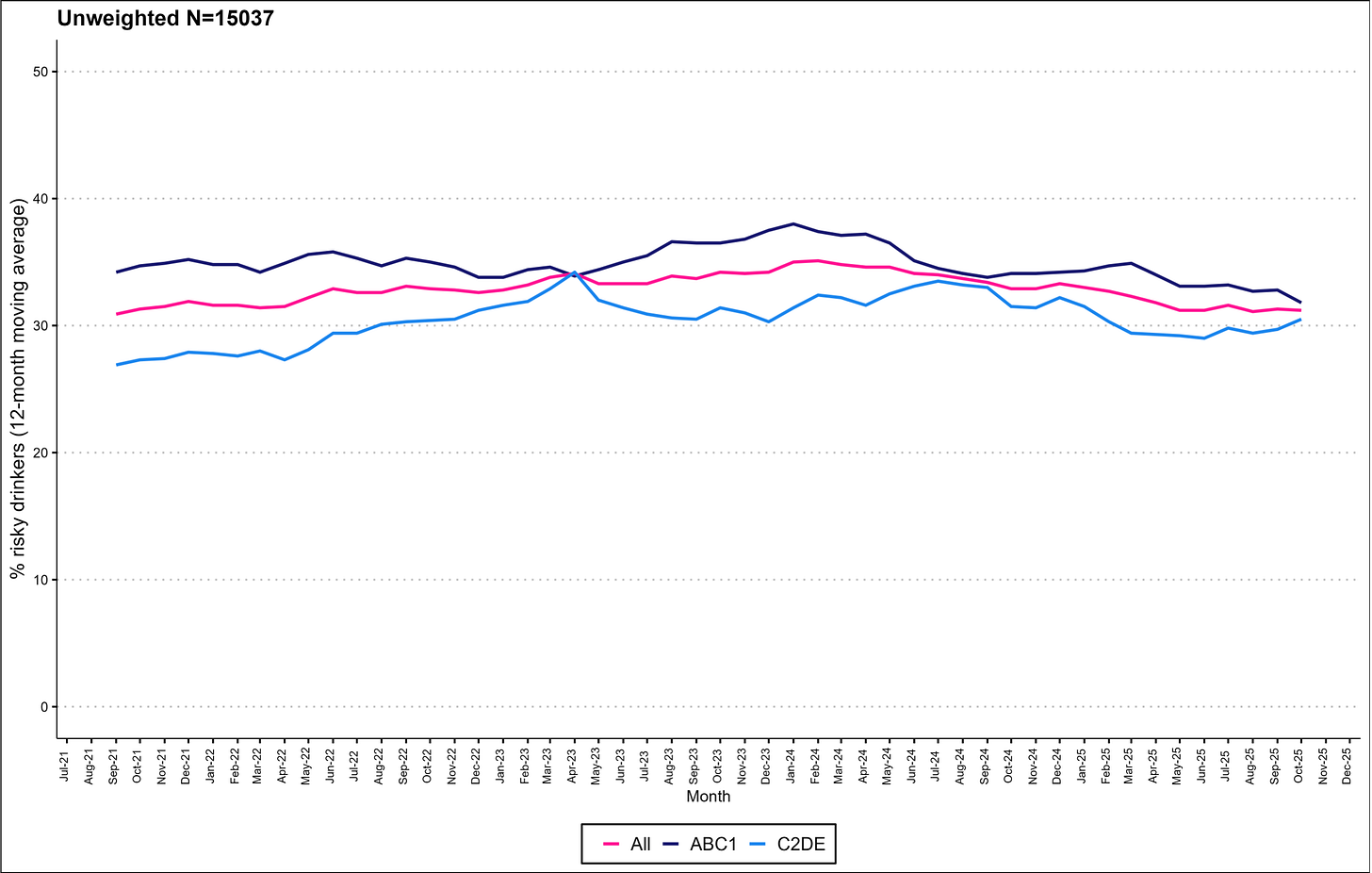
Alcohol Toolkit Study: update
The Alcohol Toolkit Study is a long-running survey of alcohol consumption in England, Scotland, and Wales. The English monthly data has been collected since March 2014, and the Scottish and Welsh data from mid-2021. Each month involves a new representative sample of adults aged 16 and over.
You can find further charts and data for each country here:
· England
· Scotland
· Wales
The following charts are a snapshot of the prevalence of risky drinking by social grade.
Prevalence of increasing and higher risk drinking (AUDIT-C)
Risky drinking defined as those scoring AUDIT-C ≥5
ABC1: Professional to clerical occupation; C2DE: Manual occupation
England
Scotland
Wales
Podcast
Our monthly podcast features interviews with experts from across the sector.
Plans to reduce drink-drive limit in England and Wales
Luca Straker –
Brake - the road safety charity

