In this month’s alert
New polling data on views regarding action on alcohol – Podcast feature
The Alcohol Health Alliance UK (AHA) has published a new report, Pouring over public opinion: Alcohol policies in the UK, analysing polling data carried out by YouGov Ltd on behalf of Action on Smoking and Health (ASH), sharing insights into how the public currently view action on alcohol, and what public support there is for policies to tackle alcohol harm.
The survey results show that:
- 55% of those who expressed an opinion (excluding don’t know) felt that the government was not taking enough action on alcohol
- 7 in 10 people want government policy to be protected from the influence of the alcohol industry and its representatives
- 76% of people thought the number of units in a product should be legally required on alcohol labels, with the majority of people supporting more and better labelling of alcoholic products overall
- Over half of people would welcome marketing regulations, especially the introduction of health warnings on marketing materials and separate display areas for alcohol and its marketing in shops
It also sets out the AHA Manifesto for policymakers, which centres around four focus areas that would have the biggest collective impact on alcohol harm:
- Protect children and support people impacted by alcohol harm
- Empower individuals and build thriving communities
- Strengthen the NHS and frontline services
- Preserve the public purse
Professor Sir Ian Gilmore, AHA Chair, said:
“The results of the YouGov survey clearly show that people in the UK want to see politicians doing more to protect their health and that of their families and their communities.
“People want the opportunity to lead healthy lives and make healthy choices but current legislation, or lack of, makes this difficult when important health information is being withheld from labels and children are being bombarded by alcohol adverts.”
The report was launched with a Parliamentary event sponsored by Dan Carden MP, where attendees heard from Mr Carden along with Shadow Minister for Public Health Andrew Gwynne MP, Baroness Jenkin of Kennington, and Professor Gilmore.
In his speech, Mr Gwynne referred to the role of alcohol industry when tackling alcohol harm, stating:
“I want the industry to do better. If they, as an industry, are advocating self-regulation, but at the same time are incentivising higher-risk drinks through placement and advertising, do not expect the next Labour government to sit on its hands.”
You can watch Mr Gwynne’s speech here.
Where next for minimum unit pricing in Scotland?
First Minister Humza Yousaf has been reported to Britain’s statistics watchdog for allegedly making “grossly misleading” claims about the health benefits of minimum unit pricing (MUP) for alcohol.
Scottish Tories have asked the UK Statistics Authority to launch an investigation into Public Health Scotland’s final evaluation of MUP, which Mr Yousaf said was “quite literally saving lives.”
Sandesh Gulhane, health spokesman for the Scottish Tories, said:
“SNP ministers view MUP as the panacea in tackling problem drinking but none of the studies to date have backed up that theory – and neither does this one, despite their desperate spinning. At best the jury is still out on whether MUP is effective; indeed, there is evidence to show it’s counterproductive as it leads some problem drinkers to forego food.”
In response, a Scottish government spokesperson said:
“Public Health Scotland used research governance processes and established scientific methods to ensure impartiality, and had their quality assessment of the papers for inclusion validated by a third party not involved in the MUP evaluation.
“The draft final report was reviewed by members of the evidence synthesis advisory group, which comprised members with a variety of relevant experience, including lived experience, experience and expertise in public health, and expertise in evidence synthesis of evidence for decision making.”
The policy has been criticised for failing to reduce consumption among dependent drinkers. However, it is thought that those with alcohol dependence are less likely to respond to price. For these groups, specialist alcohol treatment services are critical.
Net outcomes of MUP include a 3% decrease in alcohol sales, and a 13.4% reduction in alcohol-specific deaths, with the most significant reductions seen amongst heavy drinkers.
Ratio of decomposed monthly rates (Scotland:England) for wholly attributable deaths and hospital admissions, January 2012 to December 2020
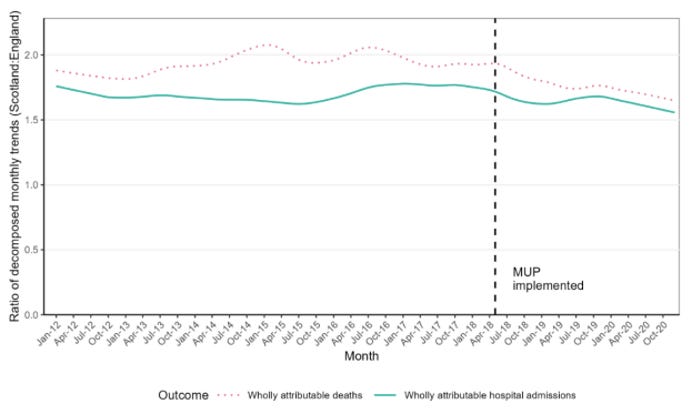
In fact, while people with alcohol dependence in Scotland participating in a qualitative interview study were sceptical about the short-term benefits for current drinkers, they felt the policy might prevent harm for future generations by reducing overall consumption.
The Scottish government is now consulting with the alcohol industry on the price of MUP in Scotland, inviting opinions on reducing the price, keeping it at 50p, or increasing it to 60p, 70p, 80p, or more than 80p.
British Medical Association motion to lower the drink-driving limit in England, Wales and Northern Ireland

The British Medical Association (BMA) has passed a motion to campaign to reduce drink-driving, calling for the limit in England, Wales and Northern Ireland to be cut from 80mg per 100 millilitres of blood, or 35 micrograms per 100 millilitres of breath, to lower levels seen in many other countries including Scotland.
Dr Katherine Severi, chief executive of the Institute of Alcohol Studies, said:
“We’ve been calling for many years for a reduction in the drink drive limit. It is nonsensical that the UK – excluding Scotland – has the unenviable title of having the highest limit in Europe.”
According to figures from the Department for Transport, there were 85,410 casualties as a result of drink drive collisions in Britain between 2011 and 2020. 2021 saw a 12-year high for fatalities from drink drive crashes, with 260 people killed during collisions, and a further 1,610 people seriously injured. Drivers with a blood alcohol concentration between 50mg and 80mg were six times more likely to die in a road traffic accident than those with zero blood alcohol.
Colin Angus, senior research fellow with the Sheffield Alcohol Research Group at the University of Sheffield, said the motion was sensible and proportionate:
“The current 80mg/100ml threshold is one of the highest in the world, at odds with most other developed nations, and higher than WHO’s recommended level of 50mg/100ml (and 20mg/100ml for new drivers). The evidence is clear that higher drink-drive limits lead to more accidents, and it’s important to remember that many of these accidents involve more people than just the drink-driver themselves.”
In order for drink-driving laws to be effective, they must be enforced appropriately. Angus highlighted that in the UK:
“police forces don’t have the power to undertake random breath tests – police need to have a suspicion that the driver is under the influence in order to test them – which goes against WHO recommendations, and there are reasons to believe that breath test numbers overall have fallen.
“If it’s a choice between lowering the limit, or not, alongside no change in enforcement, then it would still be better to lower the limit, but if we want to have the biggest impact on road safety then we need both.”
The motion commits the BMA to campaign for improved provision of specialist and community drug and alcohol services as well as a lowered drink-driving limit, two of the ten measures outlined in the BMA’s blueprint for Government to reduce alcohol-related harm.
Alcohol affordability in Ireland increased by 70% in 20 years
Alcohol on sale in shops and off-licences in Ireland is almost 70% more affordable now than it was 20 years ago, according to a new report from Alcohol Action Ireland (AAI). On-trade affordability has increased by just over 14% in the same period.
Data from the Irish Central Statistics Office was analysed by the Sheffield Alcohol Research Group. Report author, Colin Angus, said:
“The World Health Organization highlight alcohol taxes as a key tool for governments to reduce alcohol-related harm, but in order for them to be effective they need to keep pace with inflation. Alcohol duty rates haven’t changed since 2013 and recent high levels of inflation mean they are now 15% lower in real terms. This highlights the importance of linking alcohol pricing policies to inflation in order to prevent increases in alcohol consumption and harm.”
Dr Sheila Gilheany, AAI’s CEO, said:
“Affordability of alcohol is a key driver for alcohol use. Minimum Unit Pricing of alcohol is an important policy measure which we welcome. However, even with MUP, alcohol is still very affordable particularly in the off-trade sector. The introduction of MUP in Jan 2022, led to an increase in off-trade prices but this only brought them back to where they were 20 years ago.”
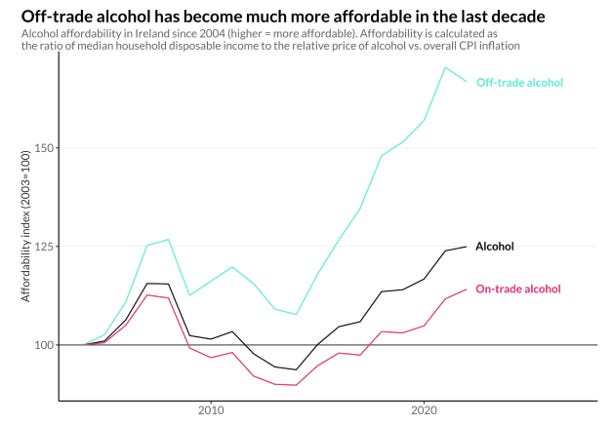
In other jurisdictions, such as Australia, there is an automatic uprating of duties in line with inflation. It is of note that the 2022 report from the Commission on Taxation and Welfare recommended that the link between the public health rationale and design of alcohol taxes should be strengthened.
Given that alcohol places a heavy burden on the health service, with 1500 hospital beds in use every day for alcohol related illness, it is vital that the government use all the policy measures at its disposal to address alcohol harm.
The alcohol industry frequently decries the level of alcohol duties in Ireland, yet in reality alcohol costs Ireland at least €3.7 billion annually while alcohol duties only raise around €1.2 billion annually. Beyond these measurable costs there is the incalculable suffering from 4 deaths every day from alcohol and the devastation to families particularly the 200,000 children impacted by alcohol harm in the home.
It is more than time for the government to have a ‘polluter pays principle’ and ensure that the alcohol industry pays for the harm caused by its products.”
What is the impact of no- and low- alcohol drinks?
Professor John Holmes, Director of the Sheffield Alcohol Research Group, is leading an NIHR-funded project investigating whether making alcohol-free or low-alcohol drinks more common and popular in the UK can improve people’s health.
Researchers from the University of Sheffield, University of Stirling and University College London, will also work closely with two specialist patient and public involvement groups involved in co-designing the research and dissemination plans.
Currently, the No/Lo Project team is developing their theory of change, and producing a timeline, which involves mapping relevant events from 2011 onwards, including product launches, marketing campaigns, industry changes, retailer actions and interventions by government and NGOs.
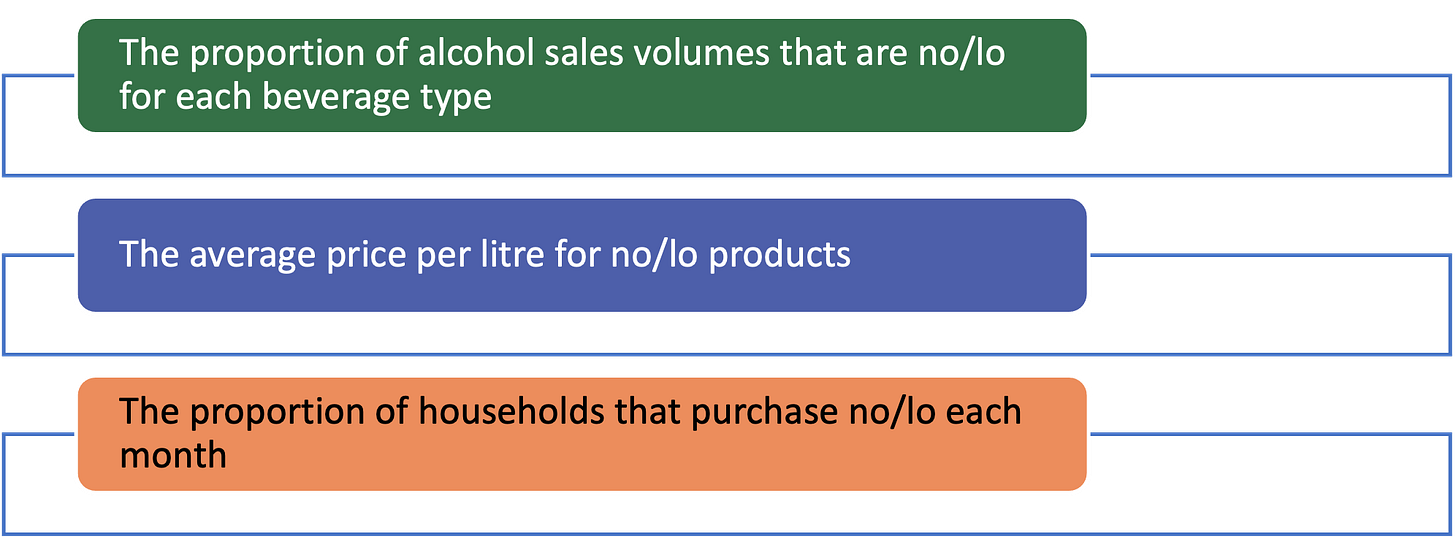
The project will describe and monitor trends in no/lo availability, sales and purchasing, assessing whether increasing no/lo consumption reduces alcohol consumption by looking at:
No/lo products have received media attention for competitive prices compared with their alcoholic counterparts. IAS chief executive Dr Katherine Severi said that brands sometimes keep the prices high as a marketing tactic:
“It can suggest to consumers that the non-alcoholic drink is ‘good quality’ and worth spending money on. Secondly, it uses the tactic of ‘prince anchoring’; latching onto the ideas consumers already have about the value to alcoholic products… And producers cash in on this assumption.
“What is concerning about the high price of non-alcoholic drinks is that they provide little incentive for consumers to try or switch to products that may help to cut down drinking rates.”
Analysis reveals 40% drop in alcohol treatment in Scotland over last decade
New analysis by Alcohol Focus Scotland shows that access to specialist alcohol treatment dropped by 40% over the last 10 years.
The number of people commencing specialist alcohol services went from 32,556 in 2013/14 to just 19,617 in 2021/22, despite the need for treatment remaining high. The drop in service provision pre-dates any impact of the pandemic on service provision, as figures prior to this still indicate a 30% decline across Scotland.
Laura Mahon, deputy chief executive of Alcohol Focus Scotland, said:
“The drop in the level of treatment in Scotland over the last ten years is shocking and deeply concerning. Alcohol harm has remained high in Scotland over this time period, so this is not a question of whether people’s need for support has reduced, but rather that they are finding it more difficult to access the support they need.
“This drop in treatment coincides with a period when budgets for Alcohol & Drug Partnerships were cut. At the time, many of us feared that those cuts would affect service provision and it now appears that is the case. The fact that this drop in support is only now coming to light is also of real concern. The Scottish Government urgently needs to invest in alcohol treatment – as they have in drug services – and to monitor provision to ensure these vital services are maintained.
“But we can’t treat our way out of the alcohol emergency – we must also prevent problems developing in the first place – which is why we also need to renew and uprate minimum unit price to at least 65p per unit, as well as restrict alcohol marketing.”
Scottish Health Action on Alcohol Problems (SHAAP) has also called for improved services following a study of alcohol frequent attenders in a West Scotland hospital (those who had been admitted to hospital for alcohol-related issues 10 times in the previous year, or three times in the previous three years.)
The report found that all participants had previously been treated for alcohol dependence, and 13 out of the 20 respondents reported experiences in their past, predominantly instances of abuse or loss. Dr Mathis Heydtmann, a consultant hepatologist and one of the report authors, said:
“A unique service dedicated to helping people with alcohol problems who repeatedly arrive at the hospital entrance would help to prevent further admissions, would reduce the strain on the NHS and would save lives.”
Dr Alastair MacGilchrist, the chair of SHAAP, said:
“This study makes clear that it is essential that people who are frequently attending hospital due to alcohol are identified as early as possible, and that a rapidly available, effective treatment service should then swing into action.
“This service should be tailored to the specific needs of this complex group, ensuring that no patient falls between the cracks of services in the future.
“The upcoming UK Alcohol Treatment guidelines should address multifaceted groups like alcohol frequent attenders specifically and must aim to mitigate against barriers which they experience in accessing treatment.”
Can governments do without public health regulation?

The Social Market Foundation (SMF) has published the first in a series of three papers exploring tobacco, alcohol, obesity and gambling policy.
These risk-factors contribute substantially to the current public health crisis: the UK government’s 2019 prevention Green Paper suggested that 40% of premature mortality can be attributed to behavioural patterns.
To tackle smoking, alcohol, obesity and gambling, policymakers attempt to alter behaviour that is often compulsive to the point of dependency, and need to reckon with a social environment that may promote harmful behaviour. This involves challenges of regulating often powerful businesses with strong economic interests at stake.
This paper compares the effectiveness of interventionist measures (such as bans and taxes) against choice-based measures (like educational campaigns) on improving public health outcomes.
SMF report that in general, more ‘interventionist’ policies (such as bans, taxes and regulations) tend to be more effective. Individual-level interventions (e.g., incentive payments and treatment services) are more amenable to experimentation, and so have stronger evidence behind them. However, the evidence on measures that affect whole populations suggests they have bigger effects and are cheaper (and so more cost-effective).
The evidence – particularly from tobacco control – suggests that a range of policies, implemented together, should reinforce one another, and make each policy more effective. Yet the most impactful measures may also be those that appear the most politically difficult, because they involve raising prices or restricting availability.
Campaigning for change in Alcohol Awareness Week – Podcast feature
Earlier this month marked Alcohol Awareness Week, run by Alcohol Change UK (ACUK) every year to raise awareness and campaign for change.
In line with this year’s theme of ‘alcohol and cost,’ ACUK published results from their survey revealing that the average drinker in the UK spends around £62,899 on alcohol over the course of a lifetime. Questions on people’s alcohol consumption revealed that 1 in 5 drinkers considered alcohol to be an ‘essential’ item in their shopping basking. This rose to 39% of drinkers considered to be at increasing risk of alcohol harm, and 65% at high risk.
Listen to our podcast to hear ACUK’s director of research and public affairs Ailar Hashemzadeh discuss Alcohol Awareness Week activities and the role of public opinion in politics.
UK government plans to grow health workforce
The government has announced that more doctors and nurses will be trained, and thousands of new roles will be created as part of a major NHS England workforce plan.
University places for medical students are set to double, a new apprenticeship scheme for doctors is planned, and medical degrees could be shortened. The government has promised £2.4bn over the next five years, setting out several targets for 2031, including:
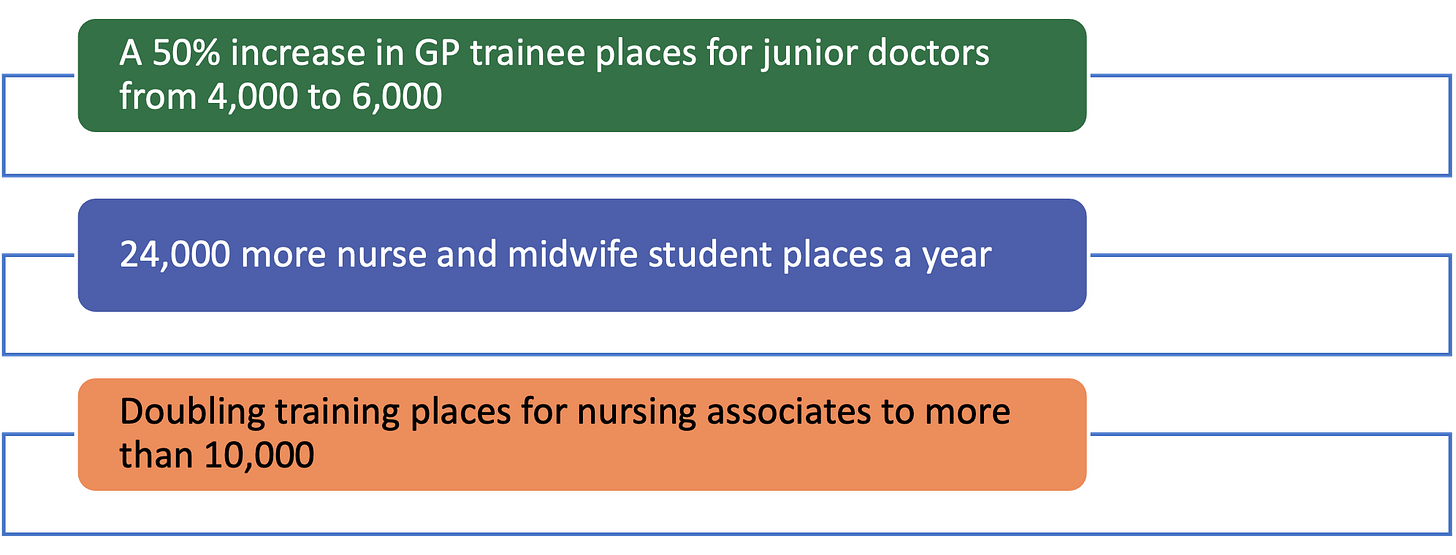
However, poor working conditions could undermine these ambitions. At present, there are more than 110,000 vacancies in the workforce, and 1 in 10 posts unfilled. With staff pay not featured in the plan, a recruitment drive will not achieve much the current staff exodus continues.
The long-term plan mentions that mental health staff should be trained in the recognition and treatment of adults and young people with co-occurring mental health and drug and alcohol use conditions, and that NHS staff should be better equipped to use screening tools such as ASSIST-Lite to identify harmful levels of alcohol and drug use. Integrated care partnerships are flagged as an opportunity to improve workforce planning, development and training for public health areas such as alcohol and drug treatment, and the 10-year drugs strategy is also highlighted.
Last year, the From Harm to hope drugs plan announced aims to rebuild the sector’s health professional workforce. The first annual report (2022 to 2023) of the drugs strategy has announced that the drug and alcohol treatment workforce has grown by 1,670 staff in the first year of funding, including more than 1,250 new drug and alcohol workers (almost 480 of whom are focused on criminal justice).
In her forward, Dame Carol Black said:
“Although encouraged by the progress made so far, I would like us to be more agile in the years ahead… Those who work in addiction need to be given appropriate resources and tools, and leaders who can bring about whole-system change.”
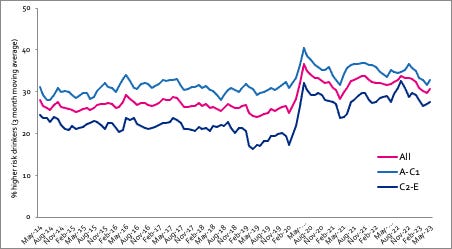
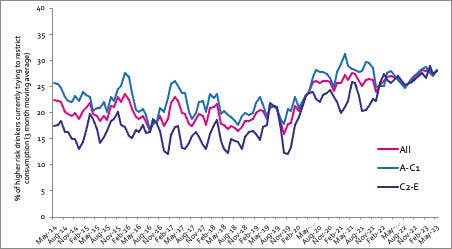
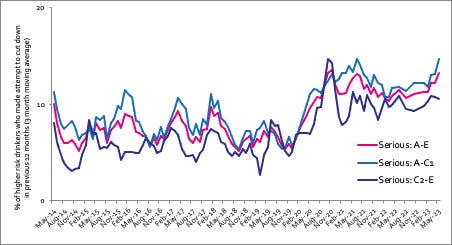
Alcohol Toolkit Study: update
The monthly data collected is from English households and began in March 2014. Each month involves a new representative sample of approximately 1,700 adults aged 16 and over.
See more data on the project website here.
Prevalence of increasing and higher risk drinking (AUDIT-C)
Increasing and higher risk drinking defined as those scoring >4 AUDIT-C. A-C1: Professional to clerical occupation C2-E: Manual occupation
Currently trying to restrict consumption
A-C1: Professional to clerical occupation C2-E: Manual occupation; Question: Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses? Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses?
Serious past-year attempts to cut down or stop
Question 1: How many attempts to restrict your alcohol consumption have you made in the last 12 months (e.g. by drinking less, choosing lower strength alcohol or using smaller glasses)? Please include all attempts you have made in the last 12 months, whether or not they were successful, AND any attempt that you are currently making. Q2: During your most recent attempt to restrict your alcohol consumption, was it a serious attempt to cut down on your drinking permanently? A-C1: Professional to clerical occupation C2-E: Manual occupation
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads

