In this month’s alert
Does the new government give reason for optimism? – podcast feature
Although the Labour manifesto lacked any policies to tackle alcohol harm, there have been a number of comments made that give reason for optimism, particularly those by Paul Corrigan – an advisor to Health Secretary Wes Streeting.
As reported by The Telegraph, Corrigan said on a recent podcast that Sir Keir Starmer could make health the responsibility of all government departments by setting up an Office for Health Responsibility. This body would prioritise health needs over other considerations – for instance changes to fuel duty. Corrigan said:
If year after year, you don’t put up fuel tax because you want to maintain petrol prices, that has an impact on health. So we can see the architecture of government that would raise health in all policies. It’s then making that happen.
The idea is modelled on a system in New Zealand and could be backed with other changes, such as each government department having a non-executive with responsibility for health.
Other reasons for optimism are the focus that senior Labour figures have on prevention, with Streeting emphasising the importance of prevention in many of his speeches. Additionally, the new public health and prevention minister, Andrew Gwynne, spoke at an Alcohol Health Alliance (AHA) event last summer where he said that Labour is considering a wide range of interventions, and a fundamental shift to focus on prevention. He also said that Labour had issued a warning to unhealthy commodity industries about how they need to reduce harm, or Labour will make them shift.
In this month’s podcast, we spoke to the AHA’s Policy and Advocacy Manager Lisa Erlandsen about reasons for both optimism and doubt that progress will be made with the new government, as well as what the AHA will be advocating for in the coming year.
Drink driving deaths rise 32% in ten years
Deaths from drink driving are at their highest since 2009, with 300 deaths in 2022. This is a rise of 32% since 2012.
The Department for Transport (DfT) states that the COVID-19 pandemic may have impacted on driver behaviour.
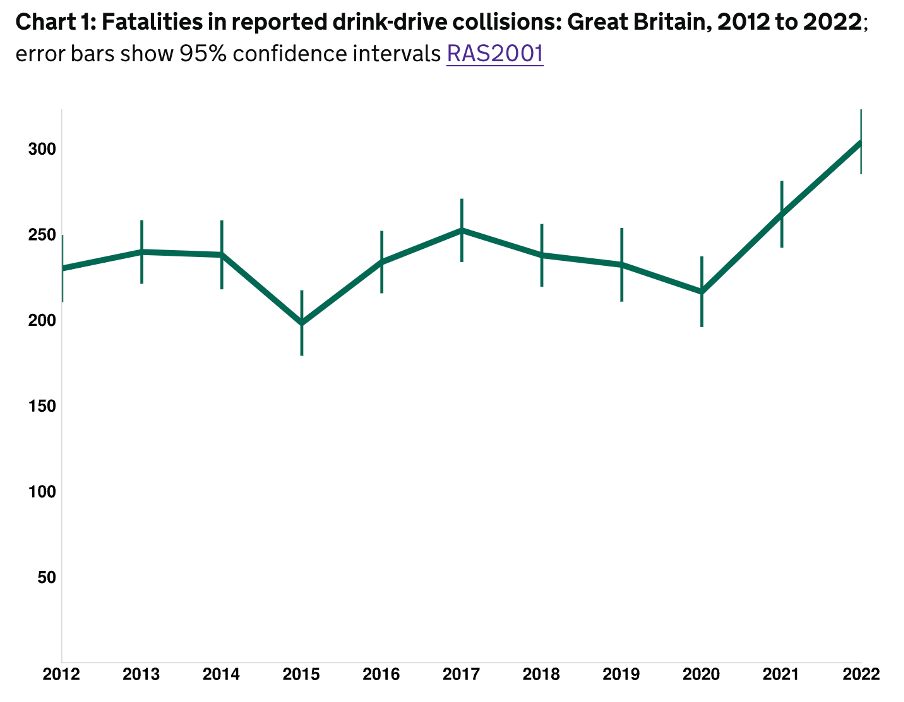
1,920 people were either killed or seriously injured (an injury for which a person is detained in hospital as an “in-patient”) in 2022, a rise of 3% since 2021. There were 6,800 casualties.
As a percentage of all traffic-related fatalities, deaths from drink-drive collisions have increased over the past two years, with 18% of all deaths being drink-drive collisions.
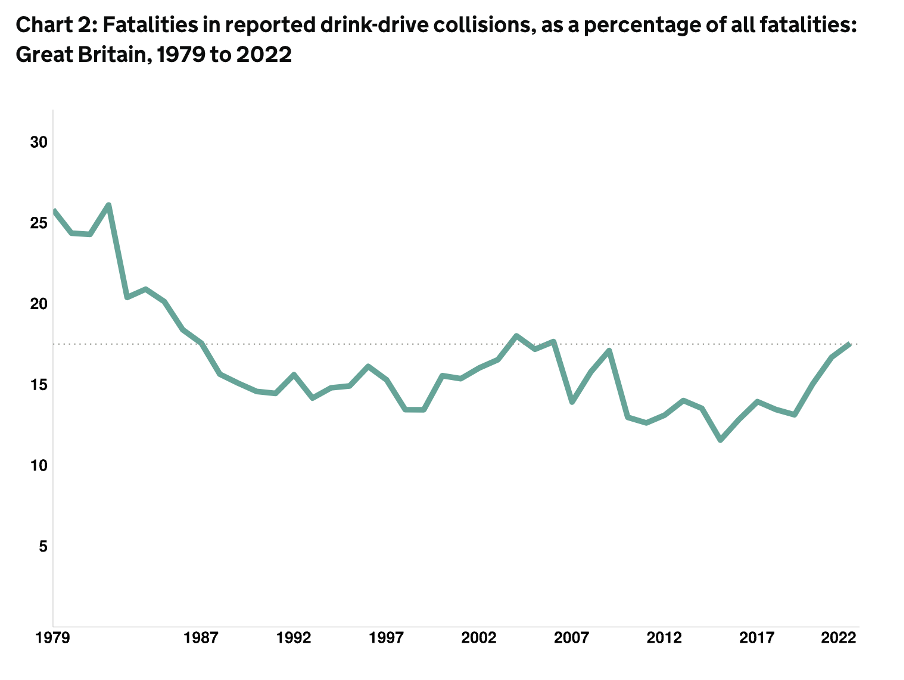
Road safety charity IAM RoadSmart called on the UK government to “give serious consideration to reviewing and reducing the drink-drive limit in England and Wales.” The limit is currently one of the highest in Europe at 80mg of alcohol per 100ml of blood, with most other countries – including Scotland – having a lower limit of 50mg.
A DfT spokesperson said that the government will deliver an updated Strategic Framework for Road Safety – the first in over a decade – to reduce deaths and injuries on the roads.
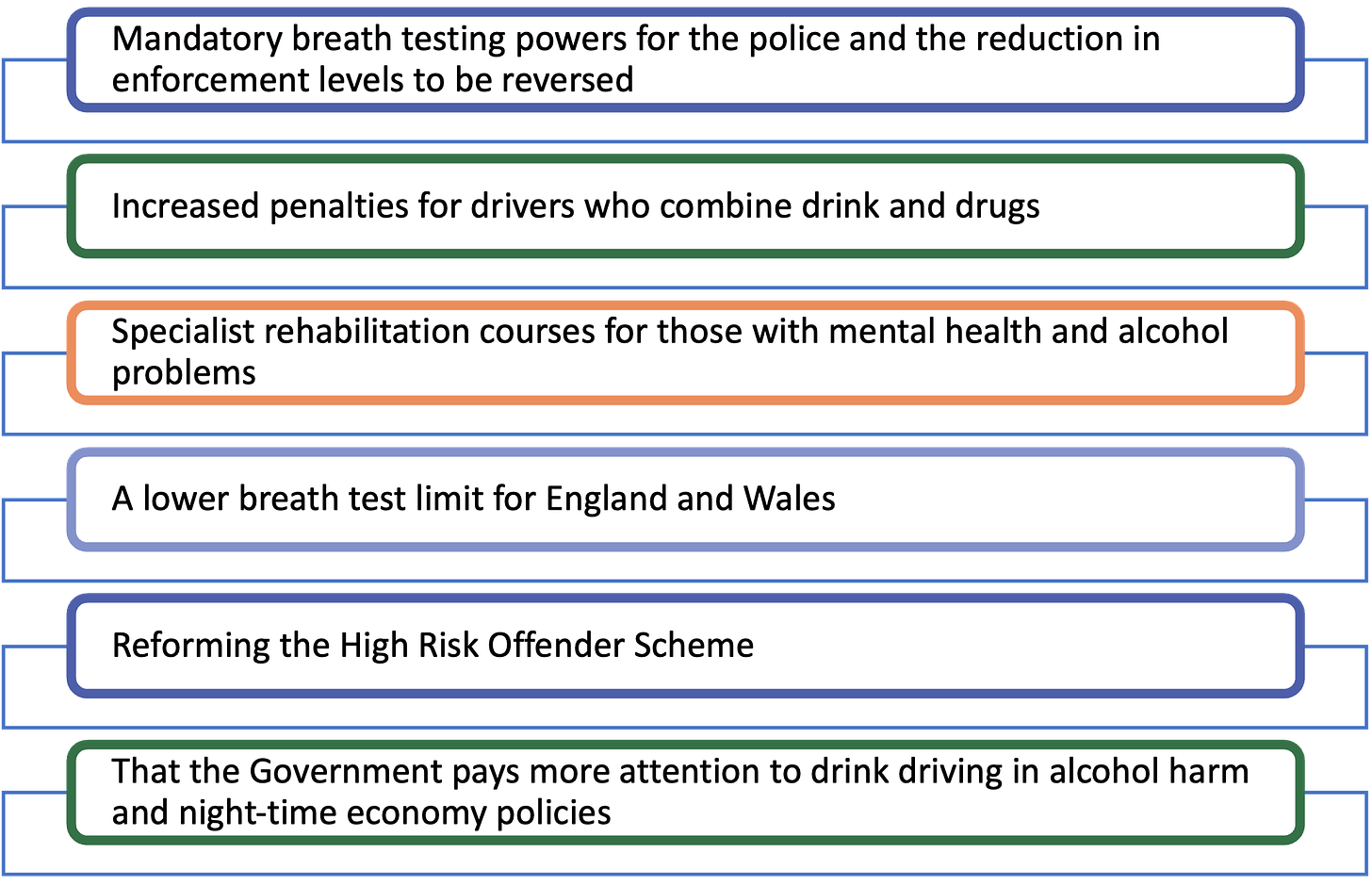
In early 2021, the Parliamentary Advisory Council for Transport Safety (PACTS) called for the government to develop a review on drink driving in order to reduce harm. Over the previous decade there had been a plateauing of deaths, after a steep fall from the early 1980s. With a rise in deaths, the report recommendations are more salient:
Little or no progress in reducing alcohol consumption and harms in Europe
Following the recent publication of its Global status report on alcohol and health and treatment of substance use disorders, the World Health Organization Europe has issued a release highlighting that very little progress has been made in reducing alcohol consumption and harm on the continent.
Dr Gauden Galea, Special Adviser to the WHO, said:
The WHO European Region continues to hold the unenviable record of having the highest levels of alcohol consumption and related harms worldwide, as well as the lowest number of abstainers. Countries need to make a strong push towards implementing the policies we know are effective in reducing alcohol consumption.
There were over 470 million current drinkers in the Region in 2019, with men consuming almost 4 times more alcohol (14.9 litres of pure alcohol) than women (4.0 litres) per year.
One in every 10 adults (11%) in the Region are estimated to have an alcohol use disorder, and almost one in every 20 live with alcohol dependence (5.9%).
However, only 12 out of 53 countries in the Region have made significant progress towards a 10% reduction in alcohol consumption since 2010, in line with the agreed targets of the NCD global monitoring framework and the European framework for action on alcohol 2022–2025.
Although the Region as a whole appears to be on track towards achieving the target, this is primarily due to substantial reductions in alcohol consumption in a few of the most populous countries, such as the Russian Federation, Turkey and Ukraine, where decisive action was taken to increase alcohol excise taxes and limit the availability of alcohol. In EU countries, however, there have been no significant changes in alcohol consumption levels for over a decade.
Scientific support for alcohol’s health benefits is fading
For centuries alcohol has been touted to provide health benefits, and modern science has somewhat supported this theory. When looking at how the amount you drink relates to your risk of cardiovascular disease, as well as all-cause mortality, studies have come up with a surprising but consistent “J-shaped curve”, suggesting that drinking a small amount of alcohol is healthier than abstaining completely.
However, as research techniques become more sophisticated, a different picture is emerging.
The Guardian published two articles on the topic, one on a specific piece of research and one on the topic in general.
In response to these studies, scientists have pointed to major methodological flaws including the number of “sick quitters” – people who have given up drinking for health reasons and the inaccuracies of self-reporting on alcohol use.
Now, a paper published earlier this year re-analysed data from previous studies and found that the lowest mortality risk was in those who had never drunk at all. As the following chart shows, lower quality studies with more bias show the J-curve, whereas studies that control for these biases better do not:
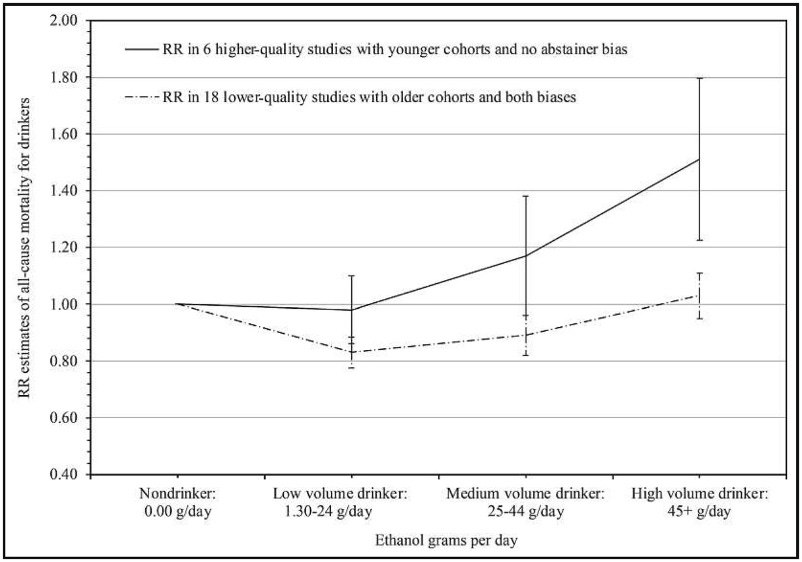
Professor Tim Stockwell, the lead author of the latest study, said that this should not be taken as a conclusive answer, rather, an indication of how much more work there is to do. He said that:
It’s more like putting up a mirror to how bad the research is.
Another recent study used a novel approach called Mendelian Randomisation, which separated people who are genetically predisposed to drink more or less alcohol, rather than relying on their self-reported drinking habits. The conclusion was simple: the more you drink, the higher your risk of developing many cancers, liver disease, stroke, and the lower your mortality.
But why does the idea of alcohol and health benefits persist in the public’s conscience? Professor Mark Petticrew, a researcher at the London School of Hygiene & Tropical Medicine, said he believed the efforts of the drinks industry explained a lot. He said:
One reason why there’s a public belief in these protective effects is because the industry has funded and promoted research, like the tobacco industry did.
Our film, Alcohol and the Heart: Explained, discusses the biases inherent in observational studies, and what better quality studies are finding.
Professor Stockwell presented at an event in April on the same topic, which can be found here.
Time to tackle the “escalating crisis” of alcohol harm
The Alcohol Health Alliance (AHA) has called on the new government to tackle the “escalating crisis” of alcohol harm if Labour is to shorten NHS waiting lists, prevent crime, reduce inequalities, and grow the economy. They highlighted that:
Perhaps the most alarming trends we have seen in recent years is the unequal distribution of alcohol harm across society. People from the lowest-income groups are significantly more likely to be adversely impacted by alcohol, despite drinking less alcohol on average than those in the wealthiest.
The alliance reiterated the criticism of the Public Accounts Committee, which stated last year that:
We are concerned that the Department [DHSC] is not taking alcohol harm sufficiently seriously. It is unacceptable that deaths from alcohol rose by 89% in the last two decades… However, despite the increase in harm there has been no alcohol-focused strategy since 2012 and the latest plans to publish one were abandoned in 2020.
The AHA calls for the new government:
to introduce a comprehensive, cross-government evidence-based alcohol strategy that follows the World Health Organization’s recommendations on marketing, availability and pricing.
Cancer warnings with pictograms on labels raises people’s knowledge of alcohol’s carcinogenicity
A paper in The Lancet by the World Health Organization’s European office looked at the effect that health warnings on alcohol labels have on people’s knowledge that alcohol causes cancer. It also looked at the perceptions of three message topics and the role of images.
The study shared an online survey that was published across 14 European countries, with over 19,000 responses. The labels used were the following:

The study found that:
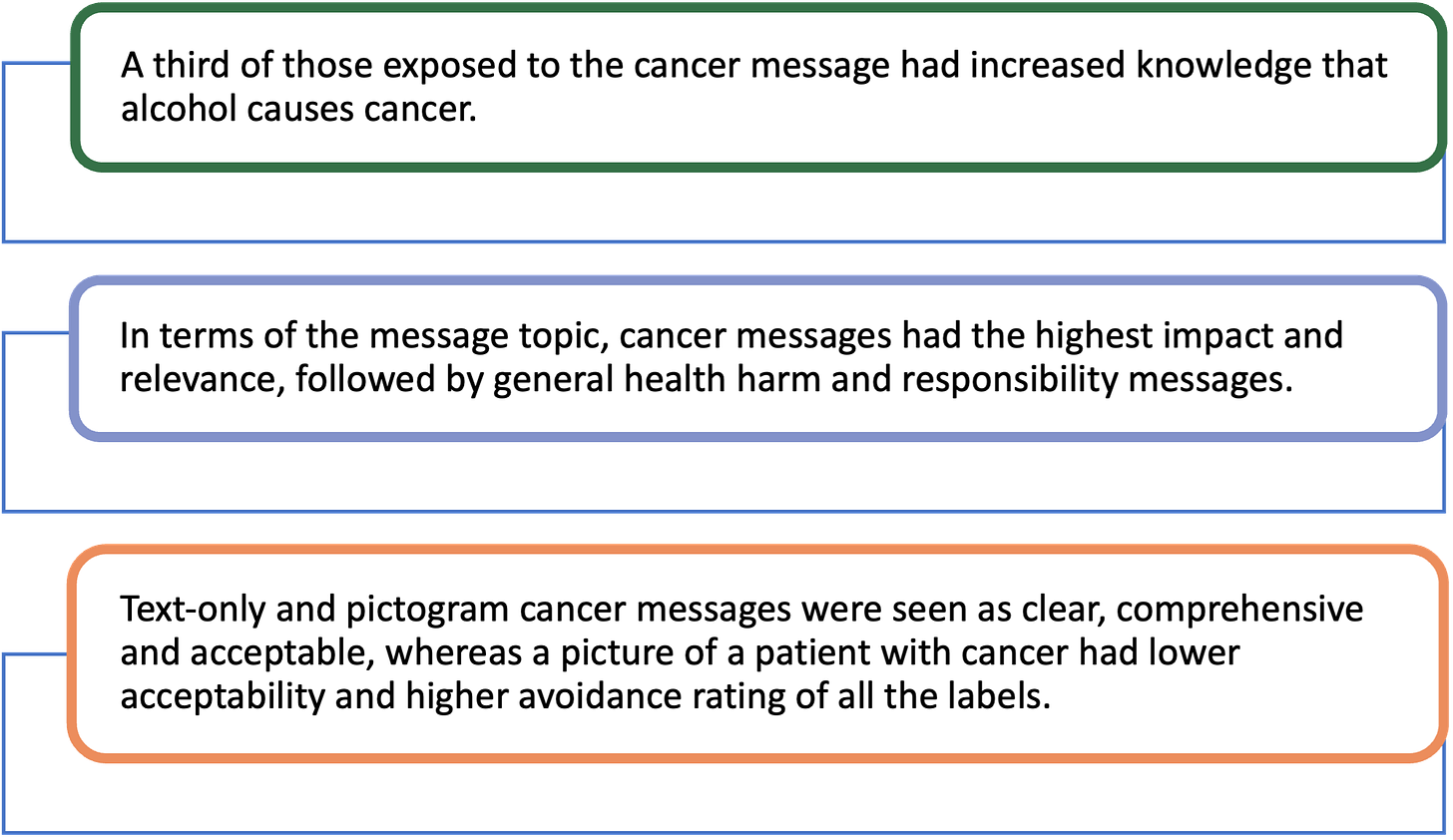
The researchers state that:
Providing such information through product labelling would reach a large number of consumers at the points of purchase and consumption, and satisfy their right to know about the harms associated with the product they are consuming.
“Above and beyond” The key role families play in recovery
My mum was dragged along by my addiction, she showed unconditional love towards me.
Adfam – the leading charity in England for those affected by someone else’s drinking, other drug use, or gambling – has launched a new report that highlights the crucial role the family plays in a person’s recovery. Over 100 people who had previously experienced problems with drinking or other drug use responded to the survey.
The report found that:
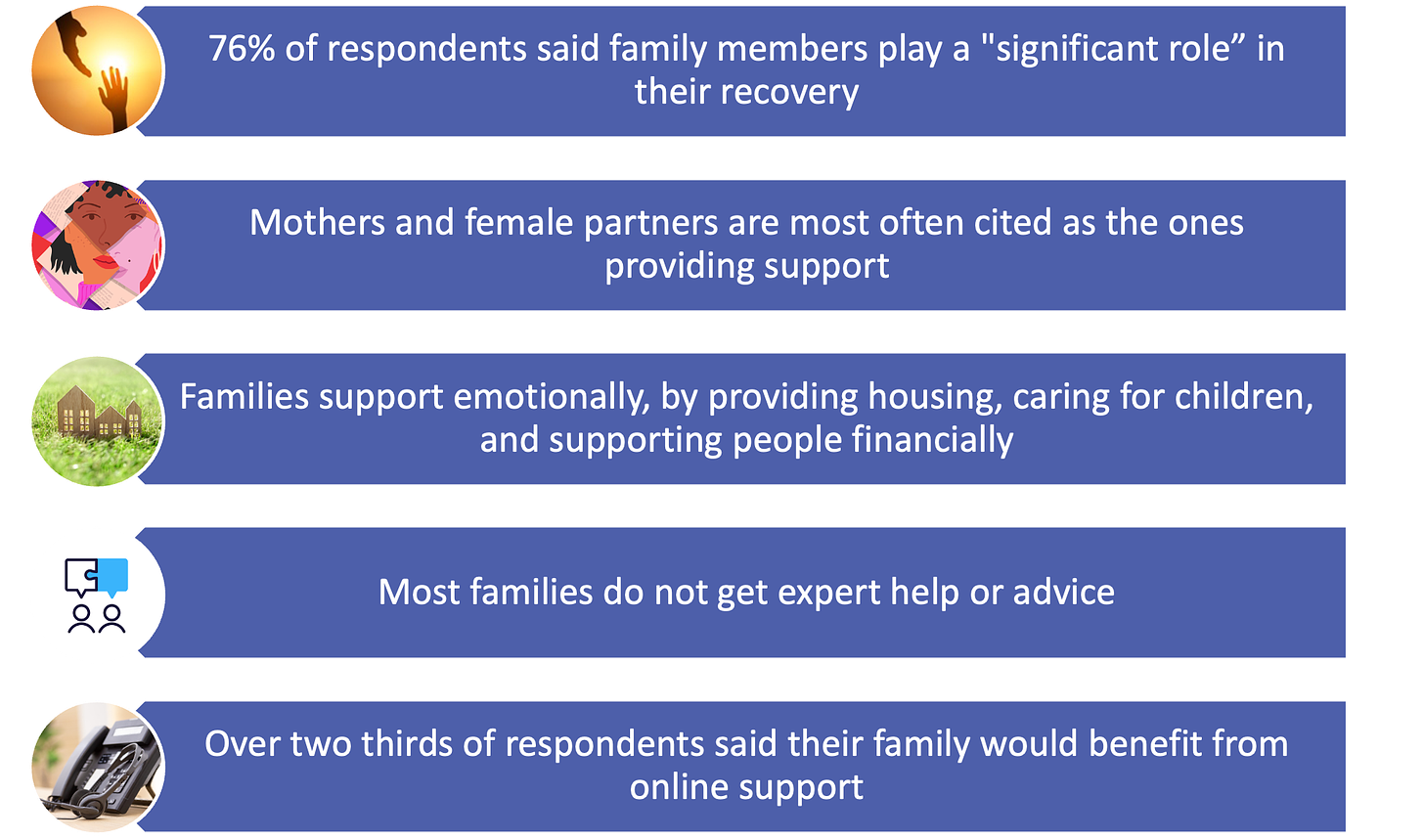
Adfam highlights that the support families give to those in recovery is likely to be a considerable financial saving to treatment services and support:
If anything approaching three quarters of [those in recovery] receive significant support from their families to help them overcome problems caused by drug or alcohol use, then that is a huge help to our drug and alcohol services and represents a massive saving to the NHS.
Alcohol Toolkit Study: update
The monthly data collected is from English households and began in March 2014. Each month involves a new representative sample of approximately 1,700 adults aged 16 and over.
See more data on the project website here.
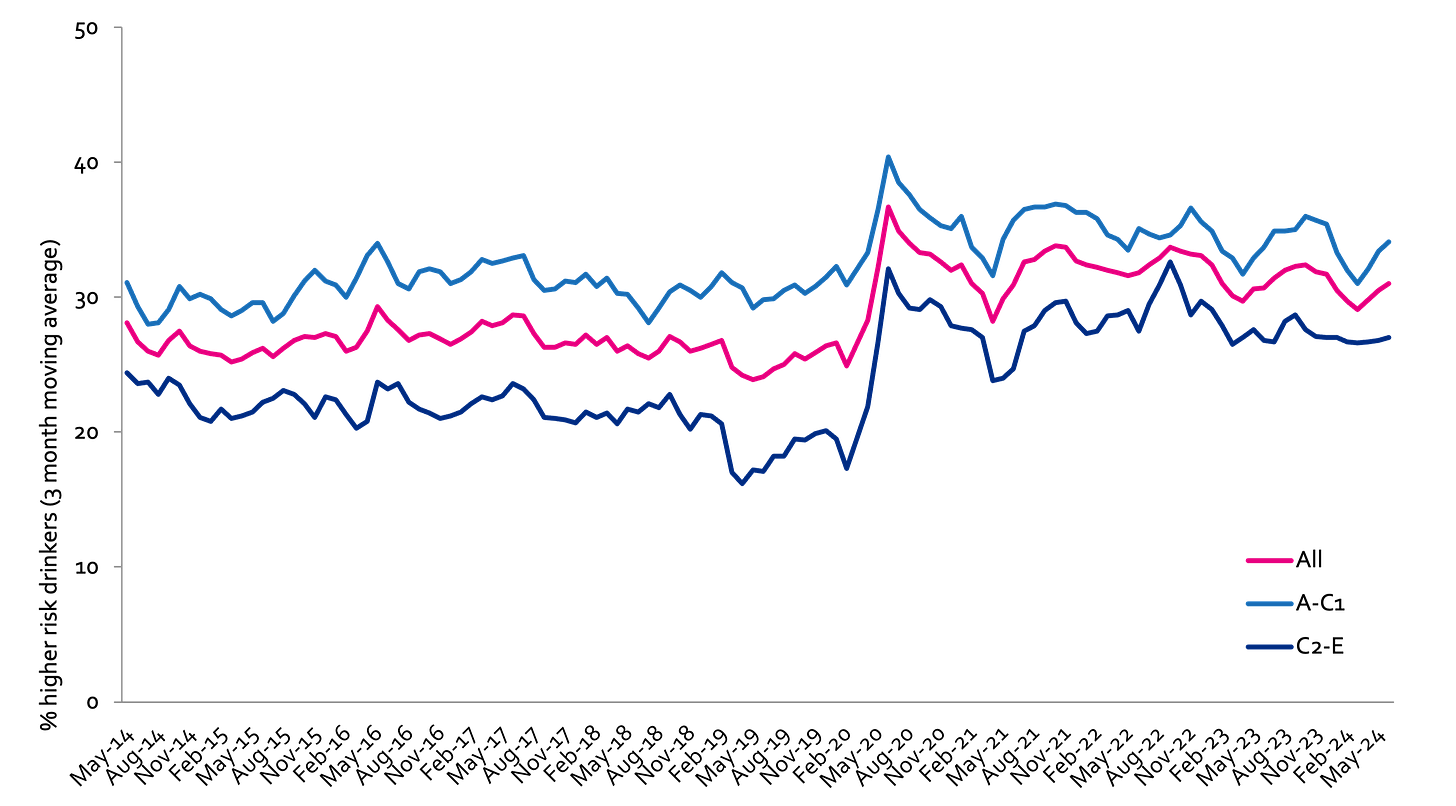
Prevalence of increasing and higher risk drinking (AUDIT-C)
Increasing and higher risk drinking defined as those scoring >4 AUDIT-C. A-C1: Professional to clerical occupation C2-E: Manual occupation
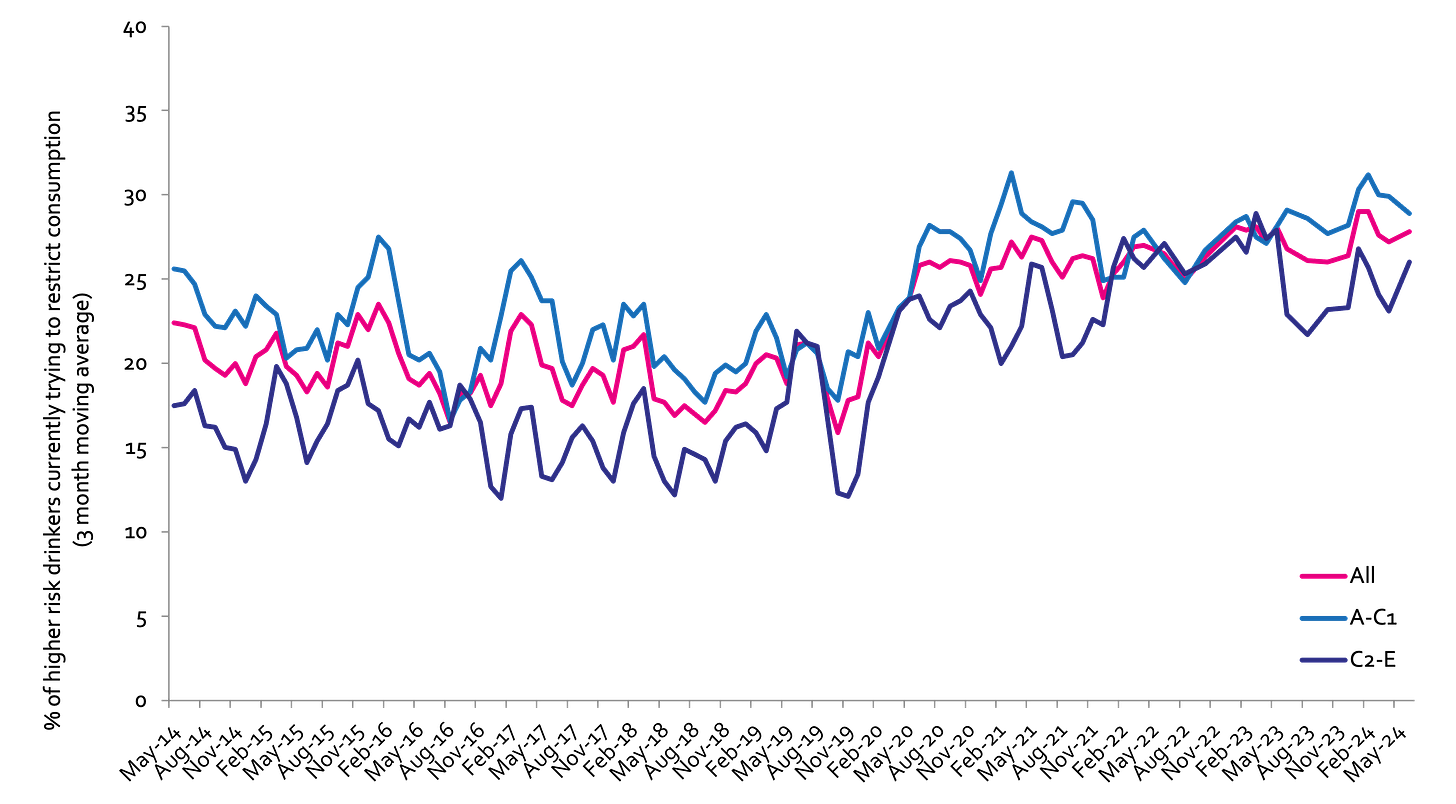
Currently trying to restrict consumption
A-C1: Professional to clerical occupation C2-E: Manual occupation; Question: Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses? Are you currently trying to restrict your alcohol consumption e.g. by drinking less, choosing lower strength alcohol or using smaller glasses?
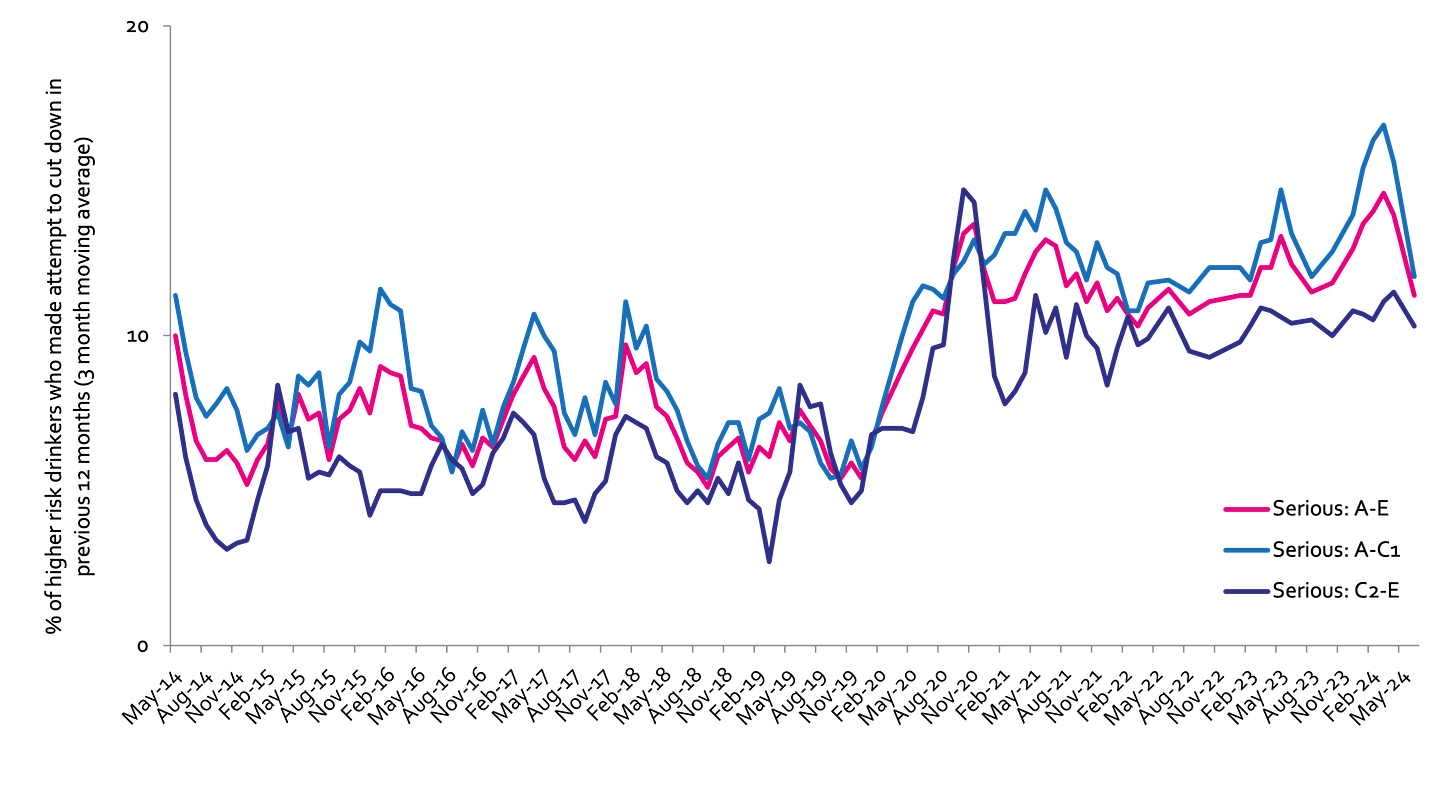
Serious past-year attempts to cut down or stop
Question 1: How many attempts to restrict your alcohol consumption have you made in the last 12 months (e.g. by drinking less, choosing lower strength alcohol or using smaller glasses)? Please include all attempts you have made in the last 12 months, whether or not they were successful, AND any attempt that you are currently making. Q2: During your most recent attempt to restrict your alcohol consumption, was it a serious attempt to cut down on your drinking permanently? A-C1: Professional to clerical occupation C2-E: Manual occupation
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads

