In this month’s alert
Editorial – November 2017
Welcome to the November 2017 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month, the Scottish Government wins its five-and-a-half year court case over Minimum Unit Pricing and signs the policy into law while the UK Government freezes alcohol duty and delays implementation of a higher duty band for white cider. Other articles include: an upward trend in alcohol mortality persists, despite revisions to official data; Alcohol Awareness Week 2017 highlights the issue of alcohol dependence; and the Alcohol Health Alliance celebrates its 10th anniversary.
Please click on the article titles to read them. We hope you enjoy this edition.
TOP STORY – Minimum Unit Pricing declared legal
UK Supreme Court ‘unanimously dismisses’ Scotch Whisky case
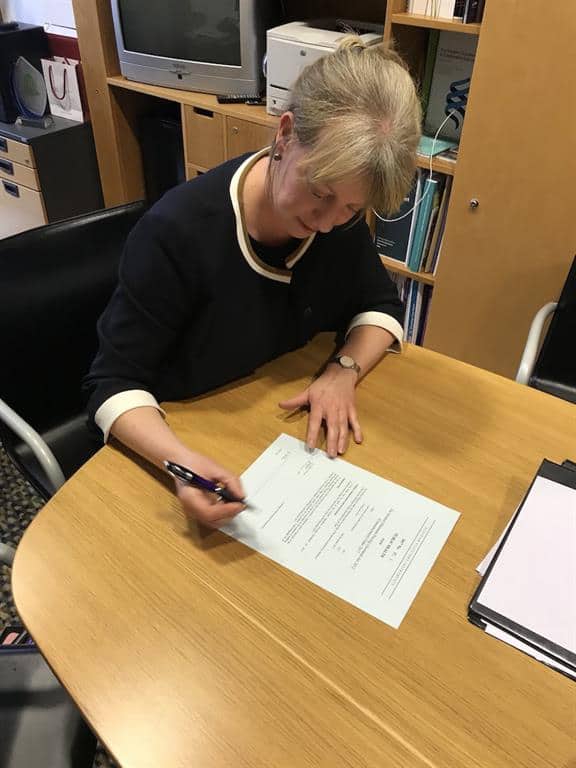
Cabinet Secretary for Health and Sport |
15 November – The UK Supreme Court delivered the final verdict on Scotland’s long running legal challenge to introducing Minimum Unit Pricing (MUP), rejecting the appeal made by Scotch Whisky Association.
The Scottish Government first passed legislation in 2012 but a number of industry bodies spearheaded by the Scotch Whisky Association (SWA) forced a series of challenges under EU law which some public health figures have described as ‘delaying tactics’.
As reported in Alcohol Policy UK, the legal challenge rested on the argument that MUP contravened EU competition law, arguing instead that taxation would be a more appropriate means of achieving its aims.
However the Supreme Court agreed with public health advocates that this was not the case and health objectives and the free market were ‘two incomparable values’, declaring MUP a ‘proportionate means of achieving a legitimate aim’. The court also rejected the appeal’s claim that the Scottish Government should have committed to going further in assessing market impact as unreasonable, acknowledging its commitments to evaluating the impacts and the five-year sunset clause.
First Minister Nicola Sturgeon tweeted:
Absolutely delighted that minimum pricing has been upheld by the Supreme Court. This has been a long road – and no doubt the policy will continue to have its critics – but it is a bold and necessary move to improve public health.
— Nicola Sturgeon (@NicolaSturgeon) November 15, 2017
Health Secretary Shona Robison also welcomed the statement, declaring the policy to be ‘a landmark moment in our ambition to turn around Scotland’s troubled relationship with alcohol.’
‘In a ruling of global significance, the UK Supreme Court has unanimously backed our pioneering and life-saving alcohol pricing policy,’ she added.
Public health groups and academics involved in MUP work took to Twitter to express relief and comment on the judgement and next steps. Chief Executive of Alcohol Focus Scotland, Alison Douglas, said of the judgment:
‘Minimum pricing is Scotland’s biggest public health breakthrough since the ban on smoking in public places. The Scottish Government are to be applauded for determinedly seeing it through in the face of global spirits producers’ attempts to deter action and delay implementation.’
Having spent over five years fiercely contesting the legislation, the SWA issued a brief statement accepting the decision and looking forward to continuing ‘to work in partnership with the government and the voluntary sector to promote responsible drinking and to tackle alcohol-related harm.’
The news was also widely covered in mainstream outlets including the BBC, The Scotsman, Telegraph, and Guardian, while many commentators speculated on the policy’s implications over the coming years. Colin Angus, one of the architects of the modelling behind the policy, defended the policy in a blog on the grounds that ‘targeting health policy at the most deprived groups is likely to see large effects’ across an entire society.
Responding to the judgement, Katherine Brown, Chief Executive of the Institute of Alcohol Studies said:
IAS response to @UKSupremeCourt judgment on minimum unit pricing pic.twitter.com/B5pVbaH0ud
— IAS (@InstAlcStud) November 15, 2017
TOP STORY – 2017 Autumn Budget: White cider tax threshold slated for 2019
Duty frozen; public health groups lament ‘missed opportunity’ on modest cider reforms
22 November – The Autumn Budget saw disappointment for public health groups, who bemoaned insufficient action on high strength ciders and a general freeze on alcohol duties.
Having announced a consultation in the March Budget, carried out over the summer, on how to tackle ‘white cider’, Chancellor of the Exchequer Philip Hammond finally revealed that a new duty rate will be applied to ciders between 6.9% and 7.5% ABV from February 2019. The Alcohol Health Alliance had called for the duty rate to cover all ciders between 5.5% and 7.5%. Moreover, Hammond did not specify the actual rate of tax on products within the new band.
The Treasury’s ‘red book’, which details the Budget measures, makes clear that the delay in implementation of the new duty rate is in order ‘to allow producers time to reformulate and lower their ABV’. If this is successful, and the strength of white cider is reduced from 7.5% ABV to 6.8%, this would mean that a 3-litre bottle of would contain 20.4 units of alcohol, compared to the 22.5 that it currently does. In the interim, tax on white ciders is actually set to fall in real terms, as inflation erodes the value of current taxes.
According to the Government, the new band is ‘carefully designed’ to mitigate the impact on traditional cider producers. Only 11.5% of the cider market is between 6.9% and 7.5% ABV, of which 78% is white cider.
However, some have objected that the reform is too limited, as it is unlikely to address the discrepancy between tax on cider and other products, illustrated by the chart below from the Institute for Fiscal Studies:
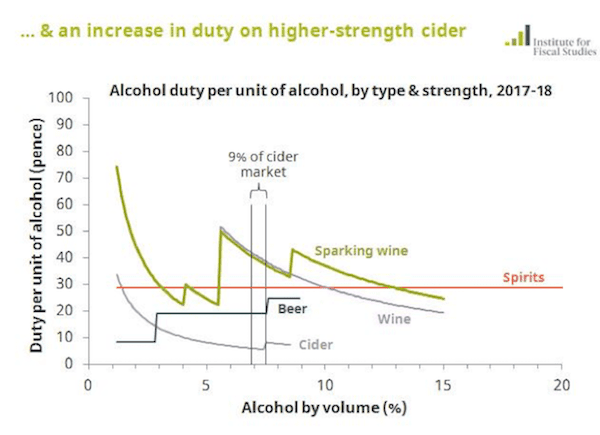
The freeze on all alcohol duties from February 2018 to February 2019 was further bad news for public health groups, as it means that the price of alcohol will fall in real terms (accounting for inflation). This is estimated to cost the exchequer £1.2 billion in lost revenue over the next five years.
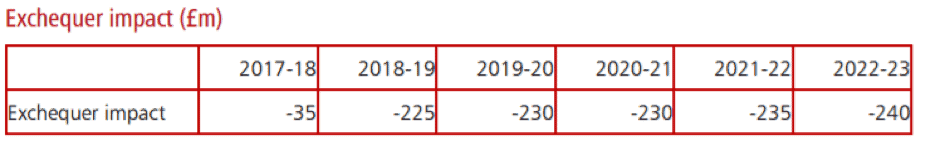
Source: HM Government, Autumn Budget 2017: policy costings |
This is the fifth year in the last six that duties have been cut or frozen, with the consequence that by 2018/19, adjusting for inflation beer duty is expected to be 16% lower than it was in 2012, cider and spirits duty will have fallen by 8% and wine duty will be 2% lower.
Prof Sir Ian Gilmore, chair of the Alcohol Health Alliance, said:
‘Today’s budget represents a huge missed opportunity for the Government to tackle alcohol harm and protect our most vulnerable…
‘The planned increase in duty on some high-strength ciders appears like a small step in the right direction. However, in reality it will have minimal impact. A three-litre bottle of white cider at the newly proposed 6.8% ABV strength will contain more than 20 units of alcohol yet could still be sold for £3.50. This will do very little to protect dependent drinkers and children that consume these damaging products.
‘Furthermore, this measure will not come into effect until 2019 and in the meantime the price of high strength cider will fall because of today’s duty freeze.
‘This strengthens the case for minimum unit pricing of alcohol. With minimum pricing now judged to be legal by the Supreme Court and Scotland and Wales moving to implement the measure, it is important that England does not get left behind in terms of reducing alcohol-related harm.’
For the most part, industry groups welcomed the news. However, some traditional cider producers expressed fears that they will be harmed by the plans. Aston Manor, producers of the leading white cider brand Frosty Jack’s issued a more robust response, accusing the chancellor of victimising poorer drinkers:
‘What this action will mean is that the vast majority of white cider consumers – not the chancellor and his friends perhaps – will be disproportionately penalised. Typically lower-income households, these “Just About Managing” [people] are lower per capita alcohol consumers.’
Such claims are at odds with an academic estimate from last year that reported cider consumption among dependent drinkers account for the vast majority of strong cider sales.
One in seven GPs turns to alcohol and drugs to cope
Adapted from Pulse magazine
From Pulse |
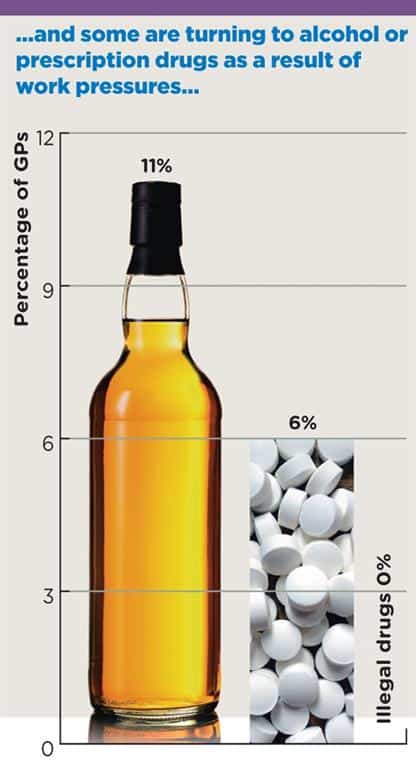
01 November – Around one in nine GPs has alcohol because of work pressures, with 6% turning to prescription drugs, a Pulse survey of more than 800 GPs has revealed.
The survey also found one in 10 GPs has taken time off work in the past 12 months because of stress or burnout, while a further 22% fear it is likely they will do so within the next year.
Around 15% of the GPs who responded to Pulse’s survey said they had turned to alcohol, prescription drugs or both to help them ‘deal with work pressures’.
One GP – who wished to remain anonymous – said: ‘I drink a bottle of wine most evenings after work, and often take codeine to help me sleep. I’m also on long-term antidepressants, as are a lot of my colleagues.’
Other respondents had similar stories: ‘I’m more likely to drink a glass of wine on a work night than on a non-work day’; ‘I started self-treating, perhaps stupidly’; ‘I’m on melatonin bought abroad to help sleep’; and ‘I don’t think I could work without fluoxetine’.
The findings follow a major University of Oxford study, published last year in The Lancet, which showed GP workload has increased by 16% in the last decade.
Former RCGP chair Professor Clare Gerada, who runs the GP Health service, said: ‘It’s worrying that one in 10 doctors go home and use alcohol to relax. That’s high. With prescription drugs, even 6% is a significant number who have expressly gone to their doctor for benzodiazepines and antidepressants to address work-related stress.’
An NHS England spokesperson said: ‘We fully understand GPs are on the front line when it comes to dealing with rising patient demand. This is why we have launched a world-first, nationally funded service to support GPs and GP trainees suffering mental ill health and addiction, while implementing measures to boost the wider primary care workforce and reduce individual GP workload.’
Almost half of pupils have tried alcohol
2016 data not comparable but higher than previous years
02 November – 44% of children have had an alcoholic drink during their school years (illustrated below), according to the new NHS Digital Smoking, Drinking and Drug Use Among Young People in England dataset, with one-in-ten (10%) claiming they had drunk in the last week, drinking an average (mean) of 9.6 units.
The figures are higher than the previous year’s (2014), but NHS Digital pointed out that they are not comparable, because of a revision made to the main survey question relating to alcohol use.
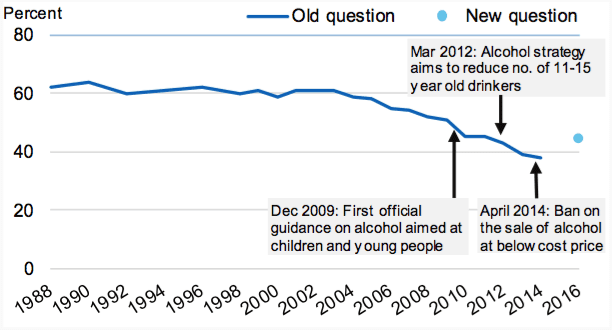 Under the old question, there was a decline in the proportion of pupils |
NHS Digital reasoned:
‘In previous years, the question used to establish whether a pupil had drunk alcohol was: “Have you ever had a proper alcoholic drink – a whole drink, not just a sip? Please don’t count drinks labelled low alcohol.”
‘Before the 2016 survey took place, the questionnaire was tested with a group of pupils and this question caused confusion.
‘In general, pupils thought the use of the word ‘proper’ meant the question referred to spirits only. They were also unaware of what would be considered a ‘low alcohol’ drink and some assumed low alcohol would include beer, cider, cocktails and alcopops.
‘In light of this feedback, the question was changed for the 2016 survey to: “Have you ever had an alcoholic drink – a whole drink, not just a sip?”’
James Morris reports in Alcohol Policy UK that ‘whilst the data suggests a significant improvement over the last 15 years as part of a trend in more abstemious younger generations, the figures prompted some speculation that the positive downward trend may be ending, albeit that further data will be needed.’
On the revised methodology, Morris observed that whilst minor, ‘the change may have impacted on subsequent questions because some of these were only asked to those pupils who answered “yes” to the initial question.’
The chapter on drinking among schoolchildren in England also found that girls (46%) were more likely than boys (43%) to report that they had ever had a drink, and to admit to having been drunk in the last week (11% compared with 9%). Beer, lager, and cider accounted for more than half the alcohol consumed by pupils in the last week.
Of pupils who obtained alcohol in the last four weeks, the most common sources were to be given it by parents or guardians (70%), given it by friends (54%), or to take it from home with permission (41%). Pupils who drank alcohol were most likely to do so in their own home (62%) at parties with friends (43%), or at someone else’s home (41%). Pupils who drank also most likely to say they drank with friends (62%) or parents (59%).
Pupils’ tolerance of drinking continues to weaken, although half of pupils (50%) still agreed that it was ok to try alcohol to see what it was like (it was 67% in 2003). Getting drunk was seen as less acceptable, with a fifth (19%) of pupils stating that it was ok to experience getting drunk, down from 31% in 2003.
New definition, same old story
Official statistics narrow take on alcohol-related mortality; deaths still trending upwards
The old (alcohol-related) criteria versus the new (alcohol-specific) |
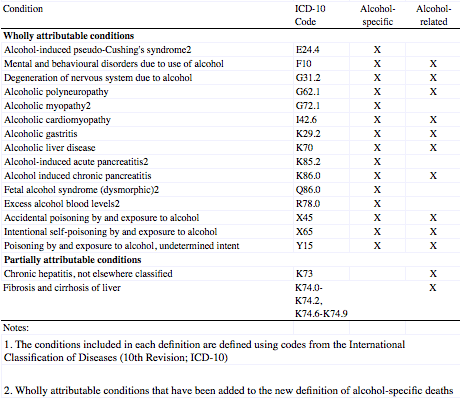
07 November – The Office for National Statistics (ONS) has released a report calculating the number of alcohol deaths in the UK in 2016, under a new ‘alcohol-specific’ measure. The figures, however, appear to tell the same old story about alcohol deaths.
In 2016, there were 7,327 ‘alcohol-specific’ deaths in the UK, an age-standardised rate of 11.7 deaths per 100,000 population. The rate of deaths remains largely unchanged since 2013, but is still higher than observed 15 years ago, the ONS says.
The statistical agency’s shift to a new standard is down to a narrowing of alcohol deaths, where each death is a direct consequence of alcohol misuse (i.e. wholly-attributable deaths).
As a result, the conditions behind these types of alcohol deaths crucially exclude unspecified hepatitis (K73) and fibrosis and cirrhosis of the liver (K74, excluding biliary cirrhosis) – as they are partially attributable to alcohol – in favour of a ‘consistent definition’ of ‘alcohol-specific’ deaths (both terms’ condition criteria are illustrated, right).
Trend data show that, although lower than the old ‘alcohol-related’ deaths, ‘alcohol-specific’ deaths are have increased at a greater number and rate over the last 15 years.
New method disputed
The narrower, ‘alcohol-specific’ definition of alcohol deaths has raised questions among public health experts, who, according to a recent editorial in The Lancet, called on the ONS in the consultation period before the change was made to do further research into the aetiology of deaths attributed to codes K73 and K74 (the latter of which accounts for the vast majority of the decrease in numbers) before discounting them entirely.
However, the ONS pressed on with the narrower definition, which was argued ‘could come at a steep cost to alcohol advocacy efforts and to the health and well-being of those affected by alcohol addiction and misuse in the UK.’
Given the dispute raised in public health quarters, it is important to remember that more complete definitions of alcohol deaths – ones that take into account partially attributable causes – are provided by the public health agencies. Public Health England’s Local Alcohol Profiles dataset estimated that almost 24,000 deaths were caused by alcohol in 2016, the Scottish Public Health Observatory estimated that around 1 in 20 (5%) of all deaths in Scotland are caused by alcohol, and in Wales it is estimated that 1,500 alcohol deaths were caused by alcohol between 2010 and 2012. A separate definition of alcohol deaths is not available for Northern Ireland, however.
The ONS admits that its new definition ‘underestimates the burden of alcohol consumption on mortality as it excludes diseases where there is evidence showing that only a proportion of the deaths, for a given cause, are caused by alcohol’, and that these definitions ‘benefit from providing a more realistic estimate of deaths caused by alcohol.’
Underlying narratives unchanged
Despite the ONS’s changes, many underlying narratives about alcohol deaths remain the same:
- The male alcohol-specific death rate continues to be more than double the rate among females
- For both sexes, rates of alcohol-specific deaths were highest among those aged 55 to 64 years in 2016
- Scotland remains the constituent country with the highest rate of alcohol-specific deaths in 2016; yet Scotland has also seen the largest decrease in its rates since they peaked in the early 2000s.
- In England, for both sexes, alcohol-specific rates in 2016 were significantly higher in the most deprived local areas when compared to the least deprived local areas.
The ONS also provided figures using the old ‘alcohol-related’ deaths definition one last time. This showed that there were 9,214 deaths attributable to alcohol in 2016, up 5% on 2015, when there were 8,758 deaths. The rate also increased from 14.2 to 14.8 deaths per 100,000 persons, driven largely by a greater rate of increase among men than women.
Charity: Parental alcohol misuse ruins children’s lives
Nearly 100 teens forced to flee troubled homes daily
08 November – Nearly 100 teenagers are made homeless each day in the UK as a result of alcohol misuse by their parents, research has shown.
Alcohol misuse among adults is damaging the lives of an estimated 700,000 teenagers across the UK, with one in four of these having been homeless in the last five years as a result – amounting to 96 per day, according to a study by The Children’s Society. The charity is now warning that as demand for council children’s services rises, cuts to local authority budgets are leaving a growing number of children struggling to deal with problems that stem from living in homes where alcohol or drugs are being misused.
The research, which surveyed 3,000 families with children aged 10–17 years, also found that two-in-five affected teenagers have lived with domestic violence, while for three-in-five the same parent is also suffering from depression or anxiety.
The analysis demonstrates that the problems teenagers face are rarely standalone, but interwoven with other serious issues. Almost a quarter (23%) of teenagers from homes plagued by alcohol misuse were also taking on caring responsibilities at home, likely to include domestic chores, taking care of siblings or nursing parents suffering from withdrawal. Adult mental health problems (59%) and longstanding illness or disability (44%) were also commonplace, indicating that adults may be self-medicating with alcohol to cope with these and other stressors in the family.
The charity is now calling on the Government to urgently address the £2bn funding gap for local council children’s services, arguing that “severe funding cuts” from central government, coupled with growing demand for council children’s services, is leaving children at risk as families reach “crisis point”.
Commenting on the findings, Chief Executive Matthew Reed said: ‘Millions of teenagers in the UK are suffering in silence with problems that would floor an adult. The hundreds of thousands of children whose parent has a drinking problem are sadly just the tip of the iceberg of children in desperate need of support.
‘Specialist services working with families to combat problem drinking, support for teenagers whose parent has mental ill health, or safe spaces for them to go when pressures at home mount, are becoming ever harder to find’, he added.
‘Without support at an early stage as problems emerge, these families can quickly reach crisis point and the risks for the children involved grow.’
Responding to the study, a Department of Health spokesperson said:
‘For many, enjoying a drink responsibly is part of their social lives and the UK Chief Medical Officers’ guidelines help adults make informed choices and reduce any health risks.
‘Although alcohol-related deaths remain stable, we are acutely aware of the impact that some adults’ drinking can have. That’s why we are looking at what further support we can provide to families to tackle alcohol harms.’
Fewer clients receiving alcohol treatment only
Public Health England says there is “work to be done” to address decline in numbers
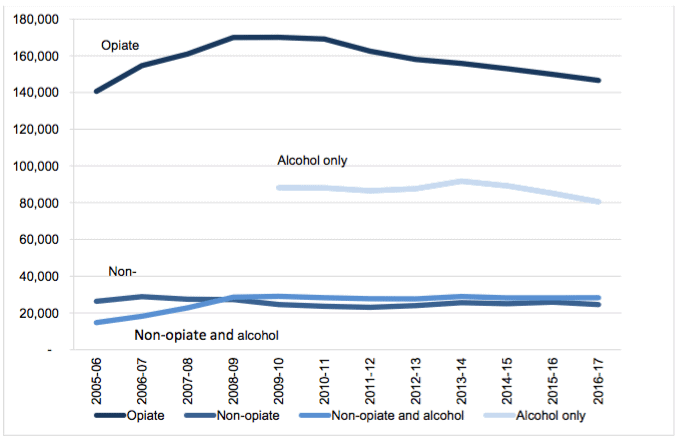
09 November – Those with alcohol dependency in England may be failing increasingly to present at clinics for the treatment they need.
This may be one reason for the fall in the number of clients receiving alcohol treatment only in the year to 31 March 2017, published by Public Health England (PHE) in its annual Adult substance misuse statistics from the National Drug Treatment Monitoring System 2016-17 report.
It found that in 2016-17, nearly 280,000 people received treatment for alcohol and drugs, a decrease of 3% and the largest drop seen over the last six years. PHE suggested that the decrease over the period is ‘largely due to the reduction in people starting treatment for alcohol problems only’ (down 5%, from 85,035 to 80,454) – the number of people getting treatment for alcohol has fallen by 12% from a peak of 91,651 in 2013-14 (illustrated, below).
Alcohol only treatment numbers compared with other substances |
Despite the fall in alcohol only treatment numbers compared with 2015-16, half of all clients in substance misuse treatment in 2016-17 (n=138,606) presented with problematic alcohol use.
Alcohol dominates the levels of new presentations to treatment in the 12 months to the end of March 2017; most new presentations to treatment in 2016-17 (60%; n=79,202) presented with problematic alcohol use, of which 52,583 cited alcohol as the only problematic substance.
The breakdown by age exposed a stark correlation – the older the patient, the more likely they were to present with alcohol use problems. The graph below illustrates that from the age of 40 onwards, most clients go for alcohol only:
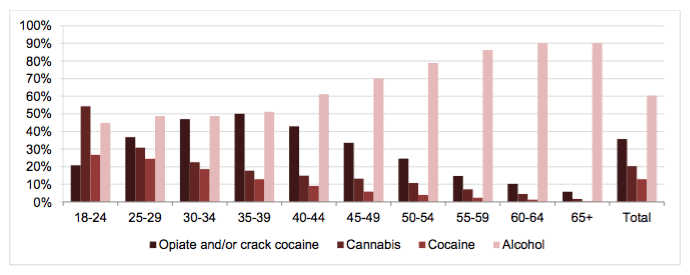
New presentations by age, 2016–17 |
Commenting on the figures in its Public Health Matters blog, PHE said:
Alcohol Awareness Week 2017
Adapted from Drink and Drugs News
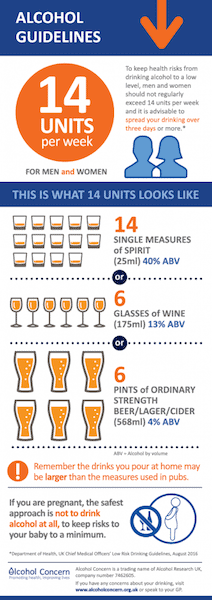
Alcohol Concern infographic |
13 November – Alcohol Concern partnered with Adfam for this year’s Alcohol Awareness Week, ‘Alcohol and Families’, running from 13–19 November. The aim was to promote ‘an honest discussion about alcohol’, particularly when it comes to the stigma that still exists around families affected by harmful drinking.
The week kicked off with an All-Party Parliamentary Group on Alcohol Harm session on families, and Alcohol Concern produced a set of free resources, including a comprehensive guide to family support services.
The number of dependent drinkers in England is estimated at around 595,000, and it’s thought that around 220,000 children are living with an alcohol-dependent adult. As well as being twice as likely to experience difficulties at school, children of alcohol-dependent parents are also four times more likely to become dependent drinkers themselves.
‘We know how few people who are alcohol-dependent actually end up engaging with services, and then obviously families are even less likely to seek help,’ says Alcohol Concern’s communications manager, Maddy Lawson. ‘Lots of people we’ve spoken to anecdotally don’t even know that there are services available. This week is about trying to get people talking about it, and to try to signpost them towards help.’
‘What we’re trying to do is raise awareness of the fact that there is family support out there – that organisations like Adfam, DrugFAM and Al-Anon are there to support people who are worried about members of their family who may be drinking too much,’ adds the organisation’s director of research and policy development, Dr James Nicholls. ‘One of the main things we’re trying to draw attention to is that people aren’t alone. One of the most common feelings is that no one else is experiencing the same things, so we want to try to raise awareness that there is support out there.’
That sense of loneliness is even more acutely felt when a loved one dies an alcohol-related death, compounding the grief by adding a profound sense of shame and isolation. In circumstances like this it’s vital for people to reach out, the charity urges.
‘The Bereaved through Alcohol and Drugs (BEAD) partnership between Adfam and Cruse has unfortunately come to the end of its funding, but one of the things that came out of that was that people really felt it was a particularly difficult experience,’ says Nicholls. ‘They felt this enormous stigma, enormous sense of guilt and enormous anxiety about how people may react, while some had experienced really problematic reactions from people around them because they just didn’t know how to respond. What came out of it was that it was incredibly important to seek support.’
The simple realisation that other people are going through the same thing can be hugely beneficial, he stresses. ‘Collectively working with each other can be really powerful in overcoming – not the pain of bereavement, because that is what it is – but certainly some of the issues around isolation and anxiety.’
‘There is support there,’ he says. ‘And the more people talk about these issues, the more people might feel comfortable about seeking that support.’
Alcohol cancer awareness rises in north east
Evidence mass-media campaigns have a positive effect
16 November – A widely publicised TV-led breast cancer campaign held in the north east of England has been found to raise awareness of the links between alcohol and cancer, according to an evaluation released in the Alcohol and Alcoholism journal. The study’s findings also suggested an increased awareness and alcohol-related policy support at a population level, but not in short-term intentions to reduce alcohol consumption.
The study involved three cross-sectional surveys; one over the fortnight pre-campaign (n = 572); one immediately following campaign wave 1 (n = 576); and another immediately following campaign wave 2 (n = 552). Survey questions assessed included: campaign exposure; awareness of the links between alcohol and related cancers; intention to change alcohol consumption; and support for alcohol-related policies.
The proportion of respondents indicating awareness of alcohol as a cancer risk factor was larger post-campaign compared to pre-campaign, with largest increase seen for breast cancer – 45% were aware of the links post-campaign (wave 2) compared to 33% pre-campaign.
The proportion of respondents indicating ‘strong support’ of the alcohol related policies significantly increased between surveys, as did the proportion of respondents both aware of alcohol as a cancer risk factor and supportive of the alcohol-related policies. However, there was no significant change in self-reported intention to reduce alcohol consumption amongst increasing/higher risk drinkers.
Alcohol rehab excluding older drinkers
Ageism may cause ‘avoidable’ deaths
21 November – A new report launched at the House of Lords has found that ageism and age discrimination in alcohol policy, practice and research is denying older people the treatment they need to recover from harmful drinking.
Published by Drink Wise, Age Well, ‘Calling Time: Addressing ageism and age discrimination in alcohol policy, practice and research’ asserts that some policies and practices are actually in breach of Equality and Human Rights legislation and calls on UK governments to develop alcohol strategies that recognise that older adults’ needs may be different to those of younger people.
Recommendations were:
- Remove arbitrary age limits for alcohol services;
- UK governments should develop alcohol strategies which incorporate age as a cross-cutting theme and explicitly recognise that older adults’ needs may be different from those of younger adults;
- Following the example of the Welsh Government, convene an advisory panel to develop substance misuse guidance focused specifically on older adults;
- Inform alcohol services of their legal obligation to provide equitable care and take action if services are consistently discriminating against older adults;
- Ensure decisions on whether or not to refer someone to rehab is made on ability to benefit. Age alone should not be a barrier to referral;
- Ensure older adults are included in clinical trials and research studies unless there is good justification for not doing so.
Higher risk drinking is declining in the UK except among people aged 50 years and older and recent figures from the Office for National Statistics underline this – older drinkers accounted for the majority of the UK’s 7,327 alcohol-specific deaths in 2016, with the highest death rate in the 55–64 age group, and there has been a 45% increase in alcohol-specific deaths in the over 50s since the turn of the century (2001).
The new report, however, states that: ‘Ageist policies can be identified easily and abolished in a relatively short period… with very little impact on resources’.
When older people do access alcohol treatment centres for rehabilitation, they are failed by the system, according to an Alcohol Research UK report ‘Accessibility and suitability of residential alcohol treatment for older adults’, released ahead of the parliamentary event.
It found that three quarters of residential alcohol treatment facilities are failing older adults because of ‘arbitrary age limits’.
Drink and Drugs News reports that more than half of alcohol rehabs on Public Health England’s online directory exclude people at the age of 66, while 75% impose arbitrary age limits of between the ages of 50 and 90 years. Older people who do access rehab may then drop out because they find the environment ‘unwelcoming or intimidating’, the report adds, with reports of ‘bullying, intimidation, and ageist language and attitudes’.
The parliamentary launch of the Drink Wise, Age Well document was led by Baroness Dianne Hayter, who wrote of the report:
‘Contrary to popular belief, harmful drinking is not the preserve of the young. In fact, many young people have followed advice and favour the gym or sports field over the pub and have been brought up never to drink and drive. Indeed, the only age group in the UK where drinking has increased is the 65–74 year-old. So our consideration – and prevention – of problem drinking has to turn to the retired, or those who’ll approach it over the coming years.
‘Drink Wise Age Well has drawn up guidance and recommendations for a swathe of organisations and professions, providing a vital tool in promoting health, happiness and a productive retirement for a growing generation.’
The event was also attended by Baroness Greengross, Lord Brooke, Lord Carlile, and Chair of the All-Party Parliamentary Group on Alcohol Harm Fiona Bruce MP among others. Speaking on the findings, Dr Sarah Wadd, one of the report’s authors and part of the Substance Misuse and Ageing Research Team at the University of Bedfordshire, noted the challenges in overcoming stereotypes associated with alcohol misuse, and raised that many of the recommendations contained in the report were free or cost-efficient.
Commenting further, Dr Tony Rao (consultant psychiatrist for South London and Maudsley NHS Foundation Trust, and the Royal College of Psychiatrists) called the document ‘a landmark report’, and raised the importance of such work in light of the baby boomer generation’s position as those most at risk of alcohol misuse. Penny Taylor, trustee of Age Scotland also raised issues associated with treating the over–50s as a homogenous group.
Dr James Nicholls, director of research and policy development at Alcohol Research UK, called the exclusion identified by the report ‘shocking’, and suggested the relatively hidden harm of home drinking might contribute to a policy focus which seems more attuned to young people’s public, predominantly night-time economy based drinking.
Finally, Caroline Phipps (director of DrugAid Cymru and chair of the Welsh Government Advisory Panel on Substance Misuse) and Thelma Abernethy of Addiction NI, spoke on the report’s findings from Welsh and N. Irish’s perspectives respectively, including referencing the need for tailored services.
Different types of alcohol elicit different emotional responses
Spirits most frequently associated with feelings of aggression, survey study shows
21 November – Different types of alcohol elicit different emotional responses, but spirits are most frequently associated with feelings of aggression, suggests research published in the online journal BMJ Open.
To explore the potential emotional factors underpinning alcohol preference the researchers drew on anonymised responses to the world’s largest online survey of legal and illicit drug and alcohol use among adults (Global Drug Survey or GDS).
The GDS, which is provided in 11 languages, includes specific questions on alcohol consumption and the feelings associated with drinking beer, spirits, and red or white wine when at home or when out.
The emotions included are energised, relaxed, sexy, confident and tired, aggressive, ill, restless, and tearful.
The final analysis included the responses of just under 30,000 (n = 29,836) 18 to 34 year-olds from 21 countries who had drunk each of the specified types of alcohol within the past year, and who had filled in all the relevant sections of the questionnaire.
Their answers showed that they attributed different emotions to different types of alcohol.
Spirits were the least likely to be associated with feeling relaxed (20%); red wine was the most likely to elicit this feeling (just under 53%) followed by beer (around 50%).
Drinking spirits was also more likely to draw out negative feelings than all the other types of alcohol. Nearly a third (30%) of spirit drinkers associated this tipple with feelings of aggression compared with around 2.5 per cent of red wine drinkers.
But spirits were more likely to elicit some positive feelings than either beer or wine. Over half (around 59%) of respondents associated these drinks with feelings of energy and confidence. And more than four out of 10 (42.5%) associated them with feeling sexy.
Responses differed by educational attainment, country of origin, and age, with the youngest age group (18-24) the most likely to associate any type of alcohol with feelings of confidence, energy and sexiness when drinking away from home.
The responses also differed by gender and category of alcohol dependency. Women were significantly more likely than men to associate each feeling–except for aggression–with all types of alcohol.
But men were significantly more likely to associate feelings of aggression with all types of alcohol, as were those categorised as heavy/dependent drinkers, who were six times more likely to do so than low risk drinkers.
And heavy drinkers were more likely to select any drink that was associated for them with feelings of aggression and tearfulness when at home or when out.
These findings suggest that dependent drinkers may rely on alcohol to generate the positive emotions they associate with drinking, as they were five times more likely to feel energised than low risk drinkers, say the researchers.
This is an observational study so no firm conclusions can be drawn about cause and effect. And the researchers emphasise that there are likely to be many factors involved in the feelings elicited by alcohol, including advertising, when and where alcohol is drunk, and the alcohol content of different drinks.
But they conclude: “Understanding emotions associated with alcohol consumption is imperative to addressing alcohol misuse, providing insight into what emotions influence drink choice between different groups in the population.”
Around 3.3 million deaths and around one in 20 cases of ill health and injury around the globe are directly attributable to alcohol.
Professor Mark Bellis, who co-authored the study, said of the findings: ‘For centuries, the history of rum, gin, vodka and other spirits has been laced with violence. This global study suggests even today consuming spirits is more likely to result in feelings of aggression than other drinks.
‘In the UK, a litre of off-licence spirits can easily be bought for £15 or less, making a double shot only 75 pence. Such prices can encourage consumption at levels harmful to the health of the drinker and through violence and injuries also represent a risk to the people around them.’
Useful research, irresponsible headlines
NHS Choices gave a damning assessment of media reporting of the study, remarking that it was ‘generally poor and in some sections, irresponsible’. It cited the Mail Online, which reported ‘Wine relaxes you, vodka gives you energy and beer boosts your confidence’, while neglecting to mention the negative emotions reported.
The Daily Telegraph came under fire for its ‘Gin really does make you more tearful than beer or wine’ headline. This statement could not be deduced from the study, as the researchers never asked specifically about gin.
The Times ran a misleading headline, saying ‘Why a tipple on a night out on the tiles raises spirits’ accompanied by a contradictory photograph of a man lying drunk on the ground.
The Guardian, however, did acknowledge the study’s limitations and said that the reasons for emotions are likely to be ‘complex’.
Ultimately, the research is useful as an initial exploration of alcohol’s impact on behaviours, but further research is needed before firm conclusions can be drawn about the subject.
Alcohol Health Alliance celebrates turning 10 years old
Campaigners awarded at ceremony held in parliament

Professor Sir Ian Gilmore addresses the audience |
22 November – The Alcohol Health Alliance UK (AHA) celebrated its tenth birthday at a special event held at Strangers Dining Room in the Houses of Parliament.
Hosted by Sarah Wollaston MP, the event saw awards given to parliamentary champions and alcohol policy advocates working to advance the organisation’s aims over the last decade. Notable winners included:
- Dr Sarah Wollaston MP (Policy Champion)
- Lord Brooke of Alverthorpe (Peer of the Decade)
- Fiona Bruce MP (MP of the Decade)
- Katherine Brown (for her contribution to AHA policy development)
- Dr Kieran Moriarty (for his longstanding commitment to the AHA)
- Balance, the North East Alcohol Office (for their campaign on alcohol and cancer)
- SHAAP and AFS (for their work to champion minimum unit pricing in Scotland)
The AHA – a brief history
Set up in 2007 by Professor Sir Ian Gilmore, then president of the Royal College of Physicians (RCP), the AHA brought together 24 alcohol and health organisations, including many of the Medical Royal Colleges, concerned about rising levels of alcohol harm across the UK.
The AHA has since grown to a membership of over 50, and is still hosted at the Royal College of Physicians, in Regents Park, London.
Over the last decade, AHA members have worked together to campaign for evidence-based measures to tackle alcohol harm and reduce the burden of alcohol on the health service. The AHA has campaigned for measures such as tax increases on the cheapest drinks, and marketing restrictions to prevent the exposure of children to alcohol adverts.
Notable steps forward in alcohol policy over the last decade include the introduction of the alcohol duty escalator in 2008, before it was scrapped in 2014, and seeing minimum unit pricing being given the go-ahead in Scotland, following a campaign from alcohol and health organisations in Scotland supported by the AHA.
Professor Gilmore has chaired the AHA since its inception. Reflecting on the past 10 years, he said:
‘We have seen plenty of ups and downs over the past 10 years in alcohol health policy. During the first few years of the AHA, we saw the alcohol duty escalator save lives and reduce hospital admissions, but were later disappointed when the escalator was scrapped.
‘We also saw the Westminster government commit to introducing minimum unit pricing, before doing a U-turn and shelving the policy.
‘However, with minimum unit pricing now going ahead in Scotland, and likely Wales, and with the Westminster government considering increasing the duty on high-strength ciders which do a great deal of harm, there are reasons to be positive about what we will achieve in the coming years.’
Professor Jane Dacre, President of the Royal College of Physicians, said:
‘We congratulate the AHA on reaching its tenth year, a testament to the hard work Alliance members have done over the past decade and their commitment to securing policy change.
‘We are proud to have set up the AHA and to continue to host the Alliance and play a leading role in its work. Our members see first-hand the damage done to health by alcohol, and by working for evidence-based measures to tackle alcohol harm, we can help prevent unnecessary death and disease, and ease the burden on our already overstretched medical workforce.’
An article, written by Professor Gilmore and AHA policy and communications officer Matt Chorley, reflecting on the last 10 years of the AHA, and what the next 10 years might bring, is available in the RCP’s Commentary magazine.
Sweden steps up efforts to ban TV alcohol advertising
Adapted from the European Centre for Monitoring Alcohol Marketing
27 November – The Swedish Government has initiated the last step in IOGT-NTO’s article 4 Audiovisual Media Service Directive (AVMSD) complaint from 2011 about alcohol advertising, which if upheld, could close the last loophole available to alcohol companies broadcasting their adverts into Sweden from abroad.
The Swedish authorities submitted a notification to the European Commission at the end of October outlining that they want to take measures against broadcasting companies advertising alcohol from countries outside Sweden, thereby circumventing the country’s domestic ban on TV advertising of alcoholic beverages.
Proper enforcement of the country’s blanket ban on TV alcohol advertising has long been hampered by its country-of-origin principle, which means that only broadcasters operating on Swedish soil are prohibited from showing alcohol advertisements.
Coming into force in 2011, the AVMSD added article 4, intended to combat abuse of the country-of-origin principle. Campaigning group IOGT-NTO launched a complaint based on the provision immediately, triggering a lengthy process in which the Swedish broadcasting authority, together with the Swedish consumer protection authority, have been pushing the European Commission to allow them to fine broadcasters for flaunting the rules.
The European Centre for Monitoring Alcohol Marketing (EUCAM) believes this case is important for public health because evidence shows that exposure to alcohol marketing, especially for minors, has a negative effect on drinking behaviour and thus public health, by increasing the amount of alcohol consumed by minors and making minors start to drink alcohol earlier.
The AVMSD sets out minimum rules with regard to alcohol advertising but states that Member States are free to adopt stricter regulation, and it for public health reasons that Sweden has stricter rules. Yet, its own rules are being circumvented.
The Commission has until 1 February 2018 to decide whether or not Swedish authorities have the right to fine the companies for breaking Swedish law or not. If the Commission says yes, it would effectively stop alcohol commercials on Swedish television and serve as a precedent for similar cases in the future.
ALCOHOL SNAPSHOT – Older drinkers more affected by Minimum Unit Pricing
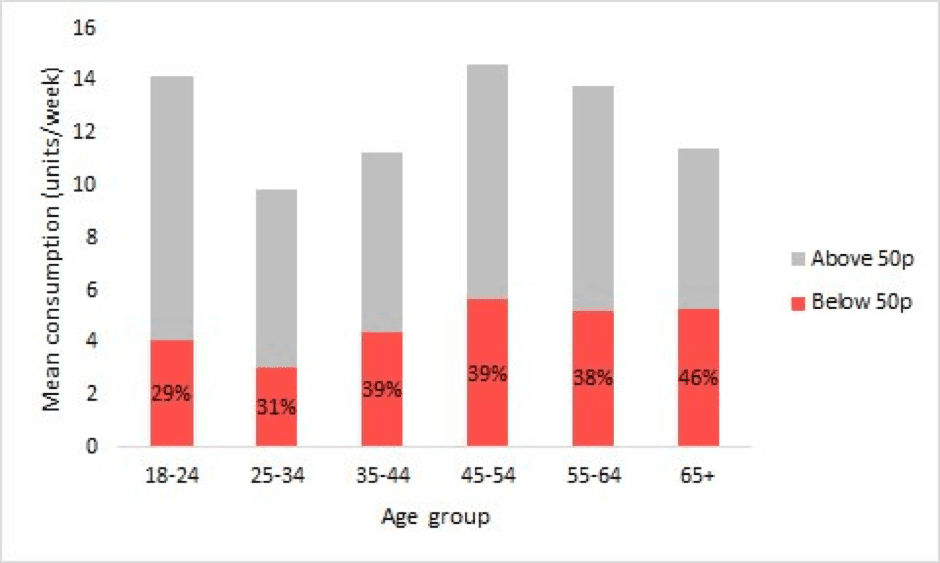 |
A common tendency in discussions of alcohol policy is to focus on the habits of younger, especially ‘binge’, drinkers as these groups are presumed to have the most harmful drinking habits. But with the recent confirmation that minimum unit pricing (MUP) will come into force in Scotland, Sheffield University’s Colin Angus took to Twitter to point out an interesting and under-appreciated fact about the distribution of the policy’s impact.
The chart above draws on data from the Scottish Health Survey and Living Costs and Food Survey to show the average number of units of alcohol consumed per week that are above and below the 50p per unit level that will be the new legal minimum. It shows that a larger share of the products consumed by older drinkers will be covered by MUP. Whereas 29% of the alcohol drunk by 18-24 year-olds is less than 50p per unit, for those over 65, the proportion is 46%. In large part, this is because younger drinkers buy more of their alcohol from pubs, clubs and bars, where prices are almost always above 50p per unit.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads