In this month’s alert
Editorial – October 2017
Welcome to the October 2017 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month, Low-level parental drinking can leave children feeling worried, according to the findings from our ‘Like sugar for adults‘ report. Other articles include: Wales introduces a minimum unit price for alcohol; fifty years after the drink-drive limit was introduced, a poll finds most drivers want it lowered; and politicians pledge to ‘Protect the Protectors’.
Please click on the article titles to read them. We hope you enjoy this edition.
TOP STORY – Report highlights childrens’ anxiety about parents’ drinking
Low-level parental drinking can leave children feeling worried
‘Like sugar for adults’ report |
18 October – Parents are more likely to cause children to feel worried around them when tipsy, a new report has found.
Published by the Institute of Alcohol Studies (IAS) in partnership with the Alcohol and Families Alliance and Alcohol Focus Scotland, “Like sugar for adults: The effect of non-dependent parental drinking on children & families” draws on data from a nationally representative online survey of almost 1,000 parents and their children, focus groups and a public inquiry involving experts and practitioners.
The report shows that parents do not have to regularly drink large amounts of alcohol for their children to notice changes in their behaviour and experience negative impacts. Having seen a parent tipsy or drunk was associated with children feeling worried as well as experiencing at least one of a range of negative impacts, including feeling less comforted than usual, facing more arguments, unpredictable parental behaviour and disrupted bedtime routines.
It also found that:
- 29% of parents reported having been drunk in front of their child.
- 51% of parents reported having been tipsy in front of their child.
- 29% of parents thought it was ok to get drunk in front their child as long as it did not happen regularly.
- If a child had seen their parent tipsy or drunk, they were less likely to consider the way their parent drinks alcohol as providing a positive role model for them – regardless of how much their parent usually drunk.
The more parents drunk, the more likely children were to experience a range of harms, beginning from relatively low levels of drinking. As a result of their parent’s drinking:
- 18% of children had felt embarrassed.
- 11% of children had felt worried.
- 7% of children said their parents had argued with them more than usual.
- 8% of children said their parents had been more unpredictable.
- 12% of children said their parents had paid them less attention.
- 15% of children said their bedtime routine had been disrupted; either by being put to bed earlier or later than usual.

From left to right: Jon Foster (IAS), Viv Evans (ADFAM / AFA), Katherine Brown (IAS), |
The launch of “Like sugar for adults” was marked by a parliamentary event led by Rt Hon Caroline Flint, MP for Don Valley (pictured, second from right). She said:
“While relatively small numbers of children reported the most worrying impacts, this study clearly shows that children know a lot about their parents drinking, and that the more parents drink the higher the likelihood of their child facing a problem. It seems likely that many parents do not realise this.
“We too quickly dismiss parental drinking as harmless fun and relaxation, but this report shows that parents do not need to be regularly drinking large amount for their children to see a change in their behaviour and experience problems. I’d like to see a more open conversation about this, among parents and professionals.”
Commenting on the report, Katherine Brown, Chief Executive of the Institute of Alcohol Studies (IAS, pictured, centre) said:
“All parents strive to do what’s best for their children, so it’s important to share this research about the effects drinking can have on parenting, and what steps parents can take to protect their children.
“Children are exposed to a barrage of marketing messages that glamourise drinking with strong links to sport and pop music. Parents have a tough job on their hands teaching children about the negative side of alcohol. Hopefully this study will help inform guidance that enables parents to make fully informed choices about their own drinking in front of their children.”
Whilst many parents strive to set a good example with their alcohol use, 15% children had asked their parents to drink less and 16% of parents reported feeling guilty or ashamed of their parenting as a result of their drinking. Children surveyed who had seen their parent tipsy or drunk were also less likely to consider the way their parent drinks alcohol as providing a positive role model for them.
The study found that positive parenting practices can protect against negative impacts experienced by children linked to drinking. A highly accessible and aware parental style reduced the likelihood of a child having asked their parent to drink less, regardless of parental consumption level.
Viv Evans, of the Alcohol and Families Alliance (AFA, pictured, second from the left), said:
“We recognise that parenting is difficult and we live in a culture which is remarkably accepting of alcohol. We hope that this study goes some way to supporting parents in a difficult job, and alerting us all to the importance of preventing problems with alcohol before they arise.”
Many studies have focused on the influence of alcohol dependence on parental skills, but this report stands apart as the first to investigate how lower level alcohol consumption impacts families in the UK – in this study, the majority of parents surveyed reported consumption levels within the Chief Medical Officer’s low risk drinking guidelines of 14 units per week.
For coverage of the parliamentary launch of the report, featuring comment from Caroline Flint MP, Jon Foster, and Viv Evans, please follow the Soundcloud link for our Alcohol Alert podcast.
Wales introduces minimum unit price for alcohol
Welsh to follow the Scots’ lead
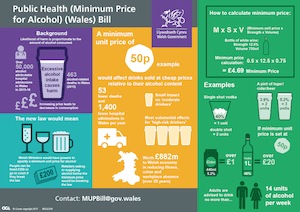
What the Welsh Government’s plans may look like for consumers |
23 October – The Welsh Government has announced the introduction of minimum unit pricing as part of its Public Health (Minimum Price for Alcohol) Bill.
The Bill will make it illegal for alcohol to be sold below a floor price per unit of alcohol consumed, as well as enable local authorities to enforce powers and bring prosecutions.
It will also address long standing and specific health concerns around the effects of excessive drinking and the availability of cheap, strong alcohol, the Welsh government said. Research has shown alcohol sold below the threshold makes up 72% of beer sales, 78% of cider sales, 42% of wine and 66% of spirits sales in Welsh off-licence shops and supermarkets.
Official figures show that there were 53,957 alcohol-related admissions of 34,932 people to Welsh hospitals in 2015/16, and 463 alcohol-related deaths in Wales in 2015. According to a Local Gov article in 2016, as much as £900m could be saved over a 20-year cycle if the unit pricing move was allowed – alongside around a reduction in 50 deaths a year.
Public Health Minister Rebecca Evans, who will bring the legislation to the Welsh Assembly, said of the Bill: “Alcohol-related harm is a significant public health problem in Wales. The 463 alcohol-attributable deaths in 2015 were all avoidable, and each of these deaths would have had a devastating effect on the person’s family and friends.
“There is a very clear and direct link between levels of excessive drinking and the availability of cheap alcohol, so we need to take decisive action now to address the affordability of alcohol, as part of wider efforts to tackle alcohol related harm.”
Will they, won’t they?
As BBC News reports, the legislation is back on the table five years after the Welsh Government first looked at introducing it. At that time, the Scottish Government was entering a legal battle against alcohol industry players led by the Scotch Whisky Association after introducing a 50 pence minimum unit price in its Alcohol (Minimum Pricing) (Scotland) Act – the UK Supreme Court is expected to give its final judgement on whether the policy can be implemented by the end of the year.
In 2014, the Welsh Government’s Advisory Panel on Substance Misuse (APoSM) concluded that the evidence shows that “the introduction of minimum unit pricing would target the most vulnerable groups in our communities and ameliorate the negative impacts of alcohol misuse.” This was supported by expert research from the University of Sheffield, which found:
- effects on health are estimated to be substantial, with alcohol-attributable deaths estimated to reduce by approximately 53 per year after 20 years, by which time the full effects of the policy will be seen
- crime is estimated to fall by 3,700 offences a year overall. A similar reduction is seen across the three categories of crime – violent crimes, criminal damage and robbery, burglary and theft
- workplace absence is estimated to be reduced by 10,000 days per year
- the total societal value of these reductions in health, crime and workplace harms is estimated at £882m over the 20-year period modelled.
Your move, Whitehall
Westminster initially boycotted the move, claiming that alcohol law falls under centrally controlled policing and criminal justice powers. But the Welsh Assembly seeks to introduce legislation on health grounds, and should the Supreme Court rule in the Scottish Government’s favour, ministers in Wales hope that a minimum unit price would become law by summer 2018.
The UK Government has also defied calls to embrace the policy in England, citing a lack of evidence, but ministers are now facing fresh pressure to change tack in the wake of the Welsh Bill.
In a letter to The Guardian, 50 signatories, including the Conservative MP Dr Sarah Wollaston and representatives of bodies including the Alcohol Health Alliance UK, urged the UK government to follow Wales and introduce minimum unit alcohol pricing in order to reduce harm and the economic cost of abuse.
The letter reads:
“We unequivocally endorse the Welsh Government’s adoption of a minimum unit price for alcohol (Wales reveals plan for minimum alcohol price, 23 October).
“Minimum unit pricing is a highly effective tool to reduce the number of deaths related to alcohol, crime and workplace absence. The Welsh Government continues to demonstrate its firm commitment to tackle the problem of cheap alcohol and the devastating effect this has on our communities, especially its most vulnerable members.
“This decisive action will not impact prices in pubs or bars but target pocket-money-priced alcohol. It is simply unacceptable that three litres of white cider, containing the equivalent alcohol of 22 shots of vodka, can be bought for just £3.49.”
GAPC2017 – Mobilising for change
Fifth Global Alcohol Policy Conference held in Australia
06 October – The Global Alcohol Policy Conference (GAPC2017), Mobilising for change: Alcohol policy and the evidence for action, was held from 4-6 October 2017 in Melbourne, Australia, hosting over 300 delegates from 40 countries.
This year’s conference maintained the tradition of focusing on advocacy, overcoming vested interests in alcohol policy development and the need for international collaboration to stop the harm caused by alcohol.
IAS hosted a pre-conference seminar series in partnership with main event sponsors the Foundation for Alcohol Research and Education (FARE), focusing on policies to tackle cheap alcohol, which provided the opportunity to showcase international evidence and advocacy expertise in support of policies that raise the price of the cheapest alcohol products which are linked to the highest rates of harm.
Other seminars held included:
- Alcohol, Gender and Family Violence Seminar – comprising presentations about alcohol and intimate partner violence (IPV) in Australia; the role of alcohol in perpetrating family violence in the Asia-Pacific region; alcohol’s harm to women and children; and whether the language of alcohol advertising reinforces gender inequality and domestic violence
- Health Promoting Hospitals – using the example of St Vincent’s hospital’s influential role in Sydney’s last drinks debate to show how hospitals can be a policy actor in promoting health
- Norwegian Sovereign Wealth Fund: Disinvestment from alcohol – the story of Norwegian NGO FORUT’s campaigning efforts in trying to persuade its narional sovereign wealth fund to withdraw its 1% stake in alcohol companies
A number of presentations addressed aspects of how the international drinks industry is pushing new markets in low and middle income countries through policy. One notable example was a presentation titled ‘Corporate enemies of science – advancing global alcohol policies in the face of unhealthy industry tactics’, which discussed the methods used by alcohol industry groups to undermine public health objectives across the globe.
The conference forged links between evidence and action, promoting the use of rigorous alcohol policy research to inform effective responses at local, state, national and international levels. The Conference Communique was presented at the final session, calling for “a re-invigorated global response to alcohol harm”, which would include:
- The development of a global binding,legal framework on alcohol harm, accompanied by a global civil society monitoring mechanism sufficiently skilled and resourced to hold Member States to their commitments;
- The inclusion of and support for healthy and effective alcohol policies in the work of regional frameworks and networks for action, and for trade agreements to permit and facilitate healthy alcohol policies; and
- A World No Alcohol Day
The GAPCs, now held biennally, have become the leading forum for the world’s alcohol policy makers, researchers, and practitioners. Melbourne, Australia was the fifth such event, following successful conferences in USA (2000), Thailand (2012), South Korea (2013) and Scotland (2015). Sri Lanka will be the host country in 2019.
The DrinkTank website has full documentation, post-event updates and videos from the conference. More information about the conference can also be found at the GAPC2017 website.
AA Ireland welcomes tougher drink-drive rules
Motoring body’s poll finds 70% of motorists in support
09 October – AA Ireland says it supports the strengthening of the drink-driving laws because it will make roads safer.
The country’s Road Traffic (Amendment) Bill 2017, introduced by Minister for Transport Shane Ross during the summer, proposes that anyone caught with a blood alcohol level of between 50mg and 80mg per 100ml will receive an automatic driving ban. Current legislation allows for a fine and penalty points for drivers below the 80mg level.
Research conducted by the motoring body earlier this year found that 70% of motorists support the proposed changes.
Some members of Oireachtas – namely from Fianna Fáil and Fine Gael, plus some Independents – are either opposed to the bill, have expressed reservations or said that they needed to look at the evidence for the change. But AA Ireland has criticised opponents of the legislation for prioritising the sale of alcohol over the safety of consumers and users and believe that Minister Ross is correct to strengthen the law and remove any ambiguity in the minds of drivers.
Speaking in the Irish Examiner, director of consumer affairs, Conor Faughnan, said Minister Ross’s bill was supported by Irish motorists and that the AA wanted to see it brought into law.
“We know that motorists support it because we asked them. Irish drivers understand the importance of the measure for improving road safety,” he said.
“Voices raised against this measure are not coming from motorists or from road safety experts. They are coming from those with a special interest in the sale of alcohol and who have not given due consideration to the impact that drink-driving has.
“AA research on drivers’ views found strong support for the proposed changes in rural parts of the country. Simply put, opponents of the provision do not speak for rural Ireland on the issue.”
Most drivers want a lower drink-drive limit
Call comes on the 50th anniversary of the limit’s introduction
10 October – An RAC survey has found that three in five British drivers are in favour of reducing the legal blood-alcohol limit in England and Wales.
The motoring group’s 2017 Report on Motoring, which sought the views of 1,727 drivers earlier this year, found that 59% of respondents are behind the idea of stricter laws to bring legislation in line with most European Union (EU) Member States (50mg alcohol per 100ml blood), or lower – 21% of those behind in favour of a lower drink-drive limit want it set at 20mg/100ml.
These findings have been released 50 years on from the introduction of the original 80mg/100ml limit, along with the breathalyser in 1967, when there were 1,640 fatalities attributed to alcohol; now around 200 fatalities occur every year as a result of drink driving.
The report suggests that fear of dangerous drunk-drivers remain a chief concern for motorists, with almost a quarter of those surveyed for the RAC Report citing this as their main worry on the roads.
In the report, the RAC writes: “With a majority of motorists wanting a lower limit, we actively supported proposals by the Northern Ireland Government on reducing the drink-drive limit to bring it in line with that of Scotland – 50mg/100ml.
“Northern Ireland is due to introduce a lower limit in 2018, but regrettably, at present it appears that the UK Government is not actively considering a change in the law.
“We continue to urge the UK Government to review the limit in England and Wales.”
Data from Police Scotland revealed that in the nine months since reducing the drink-drive limit in December 2014, the number of road offences that could be attributed to alcohol fell by 13%. When Northern Ireland plans to introduce a lower limit in 2018, England and Wales, along with Malta, will be the only EU countries left that have an 80mg/100ml limit.
The report also found that more respondents admit to driving when over the limit the morning after a heavy drinking session (10%) than shortly after drinking (8%). This figure rises to 14% for those aged under 45.
“There are still more than 5,000 accidents a year where at least one driver is over the alcohol limit, and nearly a fifth of drink-drive convictions are the morning after the night before,” said Hunter Abbott, advisor to the Parliamentary Advisory Council for Transport Safety (PACTS).
“Studies also show that if you drive while having only one-eighth of the English drink-drive limit in your system (one fifth of the Scottish limit), you are 37% more likely to be involved in a fatal accident than when sober.
“The only way to tell when you’re safe to drive the morning after is either to abstain completely or to use an accurate personal breathalyser.”
Alcohol-related deaths will go uncounted in new UK scheme
From The Lancet
26 October – On October 6, the UK’s Office for National Statistics (ONS) announced plans to revise its definition of alcohol-related mortality in an effort to unify disparate definitions currently used across the UK government. The new scheme, which uses a narrower definition of alcohol-specific (rather than alcohol-related) death, means that nearly a quarter of deaths related to alcohol misuse in 2015 will no longer be counted as such.
This narrowing definition is at odds with the increasing burden of alcohol misuse and alcohol-related harms in the UK, which disproportionately affect the most vulnerable and stigmatised populations. In 2015, there were 8,758 alcohol-related deaths in the UK, and alcohol-related hospital admissions jumped 17% between 2010–11 and 2015–16. In England – which accounts for nearly 80% of the UK’s alcohol-related mortality – a quarter of the population reports risky levels of drinking. The UK Foundation for Liver Research estimates that, if current trends continue, there will be 63,000 deaths and 4.2 million hospital admissions due to alcohol misuse in the next 5 years, at a cost to the National Health Service (NHS) of £17 billion.
These grim statistics, which derive from ICD codes, are key to informing policy and evaluating progress over time. The current national statistics definition of alcohol-related death captures those that are largely attributable to alcohol, acknowledging the well-known under-reporting of alcohol-related causes on death certificates. By contrast, the new definition will enumerate only deaths that are directly attributable to alcohol. As such, ICD-10 codes K73 (chronic unspecified hepatitis) and K74 (fibrosis and cirrhosis of the liver excluding biliary cirrhosis) will be entirely removed from the definition. For England, this change will mean a drop in the 2015 figures from 6,813 alcohol-related deaths to 5,306 alcohol-specific deaths – an instant 22% decrease.
The impetus behind the change is laudable: to harmonise the definition of deaths related to alcohol across the UK and better align them with international standards. Indeed, the existence of disparate definitions – at least four across the UK – had the potential to generate confusing statistics and conflicting messages. But the decision to adopt the narrower definition is contentious and was perhaps taken too hastily. Some of the governmental and advocacy organisations that participated in the ONS consultation process called for the ONS to do further research into the aetiology of deaths attributed to codes K73 and K74 (the latter of which accounts for the vast majority of the decrease in numbers) before discounting them entirely. But to no avail.
How this change will impact efforts to reduce alcohol-related harms in the UK is unclear, but it is not difficult to imagine how it might mitigate urgency. For example, the numbers could be used by the alcohol industry in their opposition to alcohol pricing policies, such as the Scotch Whisky Association’s ongoing case against the 50p minimum unit pricing bill (1 unit = 10mL alcohol), passed in Scotland in 2012 and currently under appeal at the Supreme Court. Similar policies – which are known to result in rapid and meaningful gains in health – are even more contentious in England, where they have yet to gain traction. One could also envision detrimental effects on funding for addiction and alcohol use disorder services in the UK, which have already been eviscerated by being split off from the NHS and by deep funding cuts.
The change in definition will also limit our ability to track changes in deaths associated with alcohol use over time. The new definition includes ICD-10-specific codes, meaning that trends can only be calculated from 2001 onward, when ICD-10 was adopted. The ONS discounted this as a major issue, however, noting that the two definitions produce similar trends from year-to-year and over longer time frames.
Data on the broader impact of alcohol on mortality will still be available for those who do their homework – the ONS will publish both definitions for one year, and will continue to calculate a wider definition of alcohol-related mortality “for information”. But in an era of sound bites and fast facts, it is likely that the top line data will get the bulk of the attention.
Harmonisation of definitions is unquestionably desirable, but the decision to adopt a new, narrower definition of alcohol-related death (due to take effect on Nov 7) could come at a steep cost to alcohol advocacy efforts and to the health and well-being of those affected by alcohol addiction and misuse in the UK. It is deeply disappointing that such an important decision – in an area of public health already fraught with contention – has been implemented with such haste.
This article was originally published in The Lancet Gastroenterology & Hepatology Editorial on 26 October 2017.
Politicians pledge to ‘Protect the Protectors’
Drunken assaults hamper emergency services, say MPs
Chris Bryant MP brought the Bill |
20 October – MPs from both sides of the House of Commons turned out in force to support the Second Reading of the Assaults on Emergency Workers (Offences) Bill 2017-19, tabled by Labour MP for Rhondda Chris Bryant.
Lasting over three hours, the debate involved MPs from both sides of the House recounting tales of emergency service workers operating in their constituencies who had complained of being threatened, harassed, and attacked by the violent behaviour of members of the public, who were sometimes said to be intoxicated.
In his address to the House, Bryant said that it should be a fundamental duty of any organisation that employs people in such circumstances to make sure its staff are safe, and that therefore, we should “adopt a zero-tolerance” attitude towards violence against staff.
This sentiment was echoed by Sandy Martin MP (Labour, Ipswich) who remarked: “If the public perceive a strong likelihood of prosecution and a stiff penalty, potential assailants, however drunk or angry they might be, will be that much less likely to launch an attack in the first place.”

Source: Alcohol’s impact on emergency services |
A 2015 IAS report into alcohol’s impact on the emergency services found that of those surveyed, three-quarters (76%) of police, half (50%) of ambulance workers, 43% of A&E consultants, and 10% of fire service workers had received an injury when dealing with drunken members of the public.
The Private Member’s Bill primarily seeks to “make provision about offences when perpetrated against emergency workers, and persons assisting such workers, and to make certain offences aggravated when perpetrated against such workers in the exercise of their duty.”
Matt Warman MP (Conservative, Boston and Skegness) and Holly Lynch MP (Labour, Halifax) also praised the Bill’s inclusion of organisations such as the Royal National Lifeboat Institution (RNLI), that often operate alongside emergency services in rescuing lives at sea.
Lynch, who recently visited the RNLI at the Tower on the Thames, said: “Predominantly, people end up in the Thames because they are under the influence of drugs or alcohol… and the RNLI meets a great deal of resistance from the people it seeks to assist. I am really pleased that we have been able to incorporate protections for it within the Bill.”
According to the IAS report, police spent more than half of their time dealing with alcohol-related incidents (53%); ambulance workers 37%, and A&E consultants and fire services spent 25% and 21% respectively.
Fiona Bruce MP (Conservative, Congleton) stressed the importance of the Bill acting as a deterrent against alcohol-fuelled incidents, such as the ones catalogued in the parliamentary inquiry she led into the impact of alcohol on emergency services (The Frontline Battle). Fiona told the House:
“We heard about police officers who were assaulted while breaking up drunken street fights, pumping the stomach of a young person and tackling house fires caused or exacerbated by alcohol-induced forgetfulness.
“I was really shocked by an account involving female police officers going into licensed premises while policing the night-time economy: ‘There is one thing that is specific to female officers and that is sexual assault. I can take my team through a licensed premise, and by the time I take them out the other end, they will have been felt up several times.’”
Bryant (pictured) presented the Bill through the ballot procedure in July as the most popular choice of six potential Bills among a survey of 40,000 of his constituents, “and around the country”. He said that its subsequent debate meant that the House was “responding to the public, which is an important part of what we are sent here to do.”
The Bill was passed without opposition and will be put to a Public Bill Committee for further discussion in due course.
Alcohol a driver of suicides in Armed Forces
New dataset shows alcohol plays huge role in mental health
10 October – This year’s annual National Confidential Inquiry into Suicide and Homicide by People with Mental Illness (NCISH) report exposes the gap between those suffering from alcohol misuse who are in treatment and those who go on to commit suicide.
England accounted for the vast majority (77%) of suicides in the general UK population (n=64,603). Between 2005-2015, the NCISH was notified of 49,545 deaths in England alone that were registered as suicide or “undetermined”, of which 13,576 deaths (27% of general population suicides) were identified as patient suicides.
In England, there were 5,954 suicides in patients with a history of alcohol misuse (45% of the total sample), an average of 541 deaths per year.
The percentage of suicides among patients with a history of alcohol misuse was higher in the other nations, although with much smaller totals:
Northern Ireland – 63% of 778 patient suicides
Scotland – 58% of 2,652 patient suicides
Wales – 49% of 817 patient suicides
Alcohol was also identified as the most common substance misused in the three months prior to suicide – 59% of patients did so, compared with cannabis (21%), stimulants (15%) and heroin (13%).
The headline figures from the report had a particular focus on the Armed Forces – between 2011-2015, 208 patients who died by suicide with mental health issues in the UK were current or former members of the Armed Forces, 3% of all patient suicides during this period.
A history of alcohol misuse was more common than in other patients, occurring in 57% of patient suicides in this group.
Professor Louis Appleby, who led the report, tweeted:
Over half patients who die by suicide have alcohol/drug misuse;, 650 deaths/yr. Only 11% are in substance misuse services. Our 2017 report.
— louis appleby (@ProfLAppleby) October 15, 2017
In all four UK countries, most patients convicted of homicide also have a history of alcohol or drug misuse, between 88% in England and 100% in Northern Ireland. According to the report, this indicates that it is unusual for mental health patients to commit homicide unless there is a co-existing problem of substance misuse.
The University of Manchester Centre for Mental Health and Safety, who conduct the annual report, wrote:
“Our findings add to the existence that much of the risk to others from mental health patients is related to co-existing drug or alcohol misuse rather than mental illness itself. This is an important message in combating stigma.
“A greater focus on alcohol and drug misuse is required as a key component of risk management in mental health care, with specialist substance misuse and mental health services working closely together as reflected in published guidance.”
Licensing figures 2017: premises called to review – why the decline?
From Alcohol Policy UK
30 October 2017 – The Home Office recently released 2017 statistics on alcohol and late night refreshment licensing in England and Wales, showing a further small but steady rise in the total number of licensed premises. Reviews of premises potentially causing problems have continued to fall significantly, though the reasons behind this are still unclear.
As of 31 March 2017 there were 211,500 premises licences, a 1% increase of 1,100 compared with 31 March 2016. The Home Office reports this is a ‘in line with the broadly increasing trend since 31 March 2008’ when 195,800 were recorded.
In addition to total licenses premises, figures also show in March 2017 there were:
- 14,300 club premises certificates, a 3% decrease of 400 compared with 31 March 2016
- 689,600 personal licences, a 6% increase of 41,700 compared with 31 March 2016
- 88,000 premises licences with late night refreshment, a 0.1% decrease of 100 compared with 31 March 2016
- 8,000 premises with 24-hour alcohol licences, the same as at 31 March 2016
On Vs off trade & saturation zones
In the last year the rise in premises were consistent across the on and off trade. Both on and off on-trade premises rose by 1% on 2016, up 300 to 39,500 for pubs, bars and restaurants, with total off-trade premises up by 400 to 54,900. A total of 81,800 premises licences are authorised for both on and off-sales of alcohol, a 1% increase of 900 compared with 31 March 2016. Last year the off-trade had risen at a higher rate of 4%, seemingly reflecting the continuing shift to off-trade consumption and closing of wet-led pubs.
Local Authorities (LAs) received 9,778 applications for new premises licences in 2016-17. Of the decisions made by March 2017, 97% (8,937) were granted and 3% (238) refused. Of these, 1,124 applications (11%) were in relation to premises within cumulative impact policies (CIPs); areas designated ‘saturation zones’ in a bid to curb further premisses where it is deemed likely to increase problems. Within the CIPs, 94% of applications were granted and 6% refused, although in 2015 we highlighted issues over previously reported CIP data questioning its accuracy and what effect they were having in practice. A study published earlier this year had found areas which had higher use of CIPs were associated with decreased alcohol-related crime rates in the period up of 2009 to 2013.
Why are reviews in decline?
In the last year 600 reviews were completed for premises thought to be causing problems aligned to licensing objectives; a decrease of 100 (14%) and a similar fall to the previous year. This represents a decline of more than 50% from 1,300 in 2010 when the data collection began. As with last year, why reviews have continued to decline significantly can only be speculated upon. Whether the continued pressure seen on Local Authority and police budgets resulting in fewer licensing roles and resources has been a significant factor is hard to determine, as is any link to the overall downward trend in violent crime.
Enforcement agencies such as police licensing roles may highlight that reviews are seen as a last resort and that engagement with premisses to address any issues should always be sought before taking formal review proceedings. Indeed the use of partnership schemes such as Best Bar None (BBN) seeking to improve responsible retailing practices have continued to grow, as have other schemes supported by industry bodies such as Community Alcohol Partnerships.
However despite claims that such schemes are effective in driving down alcohol-related crime and disorder, criticisms over a lack of robust outcome evaluations have been highlighted, as have concerns that such schemes may be seen as sufficient without the need for firmer licensing policies or national policy levers many alcohol groups wish to see. Partnership approaches have been endorsed by national government policy in which the Modern Crime Prevention strategy announced a second round of ‘Local Alcohol Action Areas’ (LAAAs) in 2016.
Reasons for completed reviews (more than one was cited in some instances) included:
- 467 were for crime and disorder, of which 93 reviews related to the sale of illicit alcohol
- 195 were for public nuisance
- 176 were for public safety
- 131 were for the protection of children
The majority of reviews (376) resulted in conditions being added to the licence or modified whilst 207 resulted in a licence being revoked or a club premises certificate being withdrawn. Eighty-eight reviews resulted in a licence or certificate being suspended whilst no action was taken following 30 reviews.
Late Night Levies and EMROS
Eight Local Authorities (LAs) reported having Late Night Levies (LNLs) in place, estimating an additional income of £1.8 million collected from fees, intended to be used by LAs and police to address the impact of alcohol on the night time economy and public services. No Early Morning restriction Orders (EMROs) have been implemented – again with claims being made that partnership working has shown its success as an alternative, although a number of LAs have sought and and failed to implement them. In 2012 the Association of Licensed Multiple Retailers announced a ‘fighting fund’ to support legal challenges against EMRO and LNL plans.
Licensing legislation: fit for purpose?
In recent years a number of reports have further questioned the suitability of the 2003 Licensing Act. Earlier this year a Lords Committee review called for a fundamental overhaul of the Act and made serious charges such as finding the ‘scandalous misuses of the powers of elected local councillors’ and the use of the Act as being ‘something of a lottery’. However Jon Foster, author of the Institute of Alcohol Studies’ (IAS) extensive 2016 report on the Act, wrote that the problems were “only half diagnosed” by the Lords review. The IAS report had recommended the introduction of a health objective and an economic objective into law, restrictions on off-trade hours and for LAs to use the Act’s options for enforcement in a more assertive manner. However national policy debates look set to focus on pricing issues for the meantime as duty announcements and a final verdict on Scotland’s long running Minimum Unit Pricing battle loom. Debates over the suitability of the current Licensing Act are still likely to return in the coming years, particularly whilst unknowns such as such steep falls in reviews remain.
This article was originally published in Alcohol Policy UK.
Wealth gap remains among Scots drinkers
Middle aged drinkers and young adults drink most
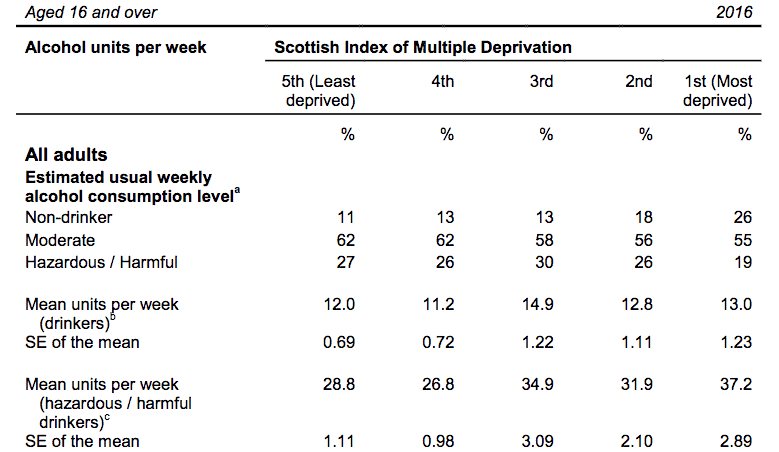
Alcohol consumption levels by |
04 October – This year’s Scottish Health Survey (SHS) shows that while consumption levels among Scots continue to plateau, the gap in hazardous and harmful drinking behaviours persists between the least and most deprived Scots.
Although the trend in hazardous and harmful drinking levels has declined significantly from 2003 (34%) to 26% in 2016, the proportion of those drinkers in the most deprived quintile in the Scottish Index of Multiple Deprivation (SIMD) is much lower than all other quintiles, with the proportion of hazardous and harmful drinkers from the least deprived areas seven to eight percentage points higher (illustrated).
Age-wise, prevalence of hazardous and harmful drinking was highest among 16-24 and 55-64 year-olds. For men, it increased from 32% among those aged 16-24 to 40% among those aged 55-64; for women, 16-24 year-olds were most likely to drink to hazardous or harmful levels (25%), followed by 55-64 year-olds (23%).
Overall, those aged 55-64 and the youngest age group (those aged 16-24) consumed the most alcohol (20.7 and 18.4 units on average, respectively for men and 10.8 and 11.3 units on average, respectively for women).
Small improvements
Compared with last year, the average number of units of alcohol consumed per week by drinkers fell a small amount, from 12.9 (2015) to 12.8 units (2016).
The proportion of adults drinking above the recommended maximum of 14 units per week in 2016 stayed level compared with 2015 (26%), and was down on 2003 (34%).
The most recently available annual estimates of alcohol sales in Scotland show that 10.5 litres (20.2 units per adult per week) of pure alcohol per person aged 16 years and over were sold in 2016 (the equivalent figure for England and Wales was 9.0 litres (17.3 units per adult per week).
Significant increases in the proportion of adults saying they did not drink alcohol were seen for both men and women over the period spanning 2003 to 2016. For all adults aged 16 and over, the percentage reporting they did not drink alcohol increased significantly from 11% in 2003 to 16% in 2013, and has remained at this level up to 2016.
Nurse-led service can reduce alcohol-related harm
Award-winning liaison service shown to improve patient outcomes
16 October – A hospital alcohol liaison service (HALS) aimed at screening all patients attending emergency departments for alcohol-related harm is the “key driver” to securing significant improvements in patient services, says alcohol specialist nurse Kerry Lyons.
Writing in the Nursing Times, Lyons, who is service lead for the Tameside and Glossop Integrated Care Organisation, explained how since 2013 the HALS operation has re-shaped the outfit’s approach to both the identification of alcohol-related harms and interventions designed to reduce them.
The aim of HALS is to have skilled teams of service providers screen all patients attending the emergency department for alcohol-related harms, ensuring specialist onward referral when necessary. HALS also prioritises a patient-led experience that reflects individual needs while reducing variability in clinical approaches.
Lyons writes that since the service was established four years ago, her organisation has been able to develop:
- Comprehensive education programmes for all staff within the trust and the community;
- An acute alcohol protocol for management of alcohol withdrawal syndrome;
- A seven-day HALS response service to all clinical areas;
- A seven-day nurse-led detoxification clinic;
- Nurse-led liver fibroscan service to assist in early identification of liver disease.
Lyons continues: “All changes were launched with an information and education cascade to all clinical staff. We followed this with regular auditing to assess and monitor compliance with these changes.
“A gap analysis was undertaken in 2013 to identify potential pathway improvement, and resulted in the launch of an ambulatory detoxification clinic in 2014 to improve patient experience and reduce hospital length of stay. The clinic is flexible and designed to respond to patients’ needs.”
As a result of the scheme, nearly 4,000 patients (including those identified as harmful drinkers) have received specialist HALS interventions and 84% of 286 patients who undertook emergency and ambulatory detoxification programmes have remained abstinent for over six months. Alcohol screening is now fully established in the emergency department for all attendees aged over 10 years. The length of stay of patients with alcohol-associated conditions has reduced from 4.7 days to 1.4 days in 2016-17 and reattendance in the emergency department for has significantly reduced. In 2016, the initiative won the Nursing Times award for Emergency and Critical Care.
HALS has been such a success story that the NHS Trust plans to develop a foetal alcohol spectrum disorder (FASD) pathway for pregnant women whose foetus is at risk of FASD, alongside an expansion of the liver fibroscan service.
WHO Europe launches SBI training manual
Adapted from WHO Europe
23 October – World Health Organisation (WHO) Europe has launched a new training manual entitled ‘WHO training on alcohol brief interventions in primary care’, aimed at supporting the development and implementation of comprehensive training for alcohol screening and brief intervention (SBI) programmes for primary health care professionals.
SBIs involve assessing a patient’s level of alcohol consumption through, for example, the Alcohol Use Disorders Identification Test (AUDIT), followed by provision of a brief intervention to motivate behaviour change.
The WHO Europe training resources form part of the Monitoring of national policies related to alcohol consumption and harm reduction (MOPAC) project, funded by the European Union.
Overview
SBIs focus on identifying individuals who are drinking at levels that may have a negative impact on their health and delivering interventions to motivate and support them to reduce or stop drinking. Such interventions vary in length, content, deliverer and delivery style, and are can complement other treatment services for alcohol dependence.
The SBI model outlined in the training materials is based on several years of experience and testing in workshops organized in Member States of the WHO European Region, and through substantial input and international expert consensus established during a series of discussions at the International Network for Brief Interventions on Alcohol and Other Drugs (INEBRIA). The training manual describes how to prepare for and set up training in SBI for health professionals in primary health care settings.
The training materials provide an overall approach to SBI implementation and skill development, which is applicable in different contexts. For the training to be relevant within specific countries, adaptations of the materials are needed. These include country-specific data on alcohol consumption and related harm, as well as the national context for the organization of the primary health care system and treatment pathways.
Furthermore, the manual outlines in detail interactive activities and role plays that form part of the training, in order to develop providers’ skills in addressing alcohol consumption with patients, as well as a section on the evidence regarding the impacts of alcohol on individual health as well as the health care system and society at large. At a systemic level, the materials also include considerations for developing training for trainers.
The rationale
The WHO Europe website states: “The need to promote evidence-based interventions such as screening and brief interventions (SBIs) has never been greater; the European Region has the highest level of alcohol consumption among all WHO regions, and alcohol-related mortality has increased over the last two decades.”
The European action plan to reduce the harmful use of alcohol 2012–2020 highlights the vital role of the primary health care system in reducing alcohol-related harm through the delivery of SBIs for alcohol. Governments can support the success of SBI programmes by ensuring that primary care providers receive the necessary training, resources and structural support. A comprehensive primary prevention approach is also key to achieving a 10% reduction in the harmful use of alcohol by 2020, as set out in the Global Action Plan for the Prevention and Control of NCDs 2013–2020.
The aim
While WHO and the wider United Nations system promote the three “best buys” of tax increases, restricted availability of alcoholic products and a ban on alcohol advertising, proactive approaches in primary health care are an essential component of a comprehensive national alcohol policy. Dr João Breda, Head of the WHO European Office for Prevention and Control of Noncommunicable Diseases, said “ensuring that health professionals are trained in addressing alcohol consumption with their patients is an important way to improve the health of individuals as well as to decrease the prevalence of disease and premature death in the population”.
Therefore, this manual has been developed to be used by Member States to expand and improve the training of health professionals on alcohol and SBI. Together with other supportive measures at the level of the health system, such training has the potential to reduce the gap between the number of people who would benefit from reducing their consumption, and the number who actually receive support or advice to do so.
As WHO Europe writes: “Now is the time to ensure that all Member States have tools to address alcohol-related problems through their primary health care systems.”
SHAAP launches guidance for treating ARLD
Good practice can help country say ‘good riddance’ to alcohol-related liver disease
Chief Medical Officer for Scotland |
24 October – The Royal College of Physicians of Edinburgh saw the launch of SHAAP’s (Scottish Health Action on Alcohol Problems) ‘Alcohol-related Liver Disease: Guidance for Good Practice’, a report providing advice for health services, local authorities, criminal justice services and the voluntary service sector to ensure consistency in approaches to prevention, treatment, care, support and recovery across the country.
Liver disease is one of the few major causes of premature mortality that is increasing, and deaths from liver disease have reached record levels. Mortality rates from Alcoholic Liver Disease (ALD) in Scotland have tripled since 1981, and in 2016, ALD accounted for 58% of all alcohol-related deaths in Scotland whilst hospital admissions for ALD have more than quadrupled since 1981/2. Treatment for alcohol-related conditions in Scotland costs over £1m a day.
The report was produced by clinicians, academics and health professionals specialising in liver care and/or public health, and put to a national consultation in 2016. Report recommendations include the following:
Specialist alcohol services should prioritise patients with evidence of alcohol-related liver damage for intervention. Services should actively, repeatedly and assertively engage with clients with alcohol-related liver damage;
Patients admitted to hospital with alcohol-related liver failure should be managed immediately, in accordance with national guidelines, be reviewed by a physician with expertise in liver disease and be engaged with an alcohol treatment service prior to discharge;
Health Boards and Integrated Joint Boards should facilitate the organisation of services to allow the operation of the care pathway recommendations.
Commenting on the launch, Dr Catherine Calderwood, Chief Medical Officer for Scotland (pictured), said: “I am delighted to be opening this important event. Alcoholic liver disease is a major cause of premature death in this country, and modelling data has shown that interventions to reduce alcohol consumption in these patients would be highly effective. This is a package of interventions that if implemented across the health service, could save the lives of patients who are most at risk of liver disease.”
Dr Eric Carlin, Director of SHAAP, said: “Problematic alcohol use continues to harm the health and living conditions of many people across Scotland. As well as emphasising the need for evidence-based approaches to reduce population consumption, most notably Minimum Unit Pricing (MUP), it is essential that service providers have access to good practice guidance to join up prevention, treatment, support and recovery approaches. This is especially important in times of financial constraint.”
Podcast
Our monthly podcast features interviews with experts from across the sector.

