In this month’s alert
Editorial – October 2018
Welcome to the October 2018 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month, Chancellor Philip Hammond leaves public health experts with a bitter taste after he freezes spirits, beer and cider duties in his Autumn Budget. Other articles include: a study finds increasing numbers of young people abstaining from alcohol; Alcohol Charter published by cross-party parliamentary group; and Ireland passes historic Public Health (Alcohol) Bill.
Please click on the article titles to read them. We hope you enjoy this edition.
COVER STORY – Budget freeze on beer, cider and spirits tax
Move to cost Treasury over £9bn in the decade to 2022/23
29 October – Chancellor of the Exchequer Philip Hammond has announced that beer, cider, and spirits duties will be frozen in this year’s Budget.
HM Treasury forecasts the move will cost the government £35 million in the fiscal year to 2019, and a further £880 million between 2018/19 and 2023/24.
This measure freezes duties on spirits, beer, still ciders and sparkling ciders below 5.5% Alcohol by Volume (ABV). This measure will be effective from 1 February 2019 for a one-year period. This means that beer duty will be 18% lower, spirits duty 10% lower, and cider 11% lower in real terms (ie after inflation) when these changes come into force than in 2012. Duty on most wine and higher strength sparkling cider will rise by retail price index (RPI) inflation.
The new band for still ciders rated at between 6.9% and 7.5% ABV – announced by the government in the Autumn Budget 2017 – will also come into effect, although it will mean the duty on cider within that threshold will rise by a mere 0.1 pence per unit at the low end (from 5.4p to 5.5p) and 1.4 pence per unit at the top end (from 5.4p to 6.8p).* The introduction of a new threshold is partly intended ‘to encourage reformulation to lower ABV levels of cheap, high strength ‘white ciders’ associated with problem drinking.’ However, if white cider makers do reformulate down to below 6.9% ABV as anticipated, it will reduce the alcohol content of a three-litre bottle by only 2.1 units (from 22.5 units to 20.4 units).
The cumulative impact of duty cuts will be £1.2 billion in 2019/20, and £9.1 billion in the 10 years to 2022/23.
The announcement follows representations made to the MP for Runnymede and Weybridge from Conservative Party colleagues, and in particular a sustained lobbying campaign from Scottish members of the party. He told the House:
‘I have received numerous representations from my right hon. and hon. Friends on one particular subject, and in response I will be freezing beer and cider duty for the next year, keeping the cost of beer down for patrons of the great British pub.
‘And in response to the concerted lobbying of my Scottish Conservative colleagues, I will also freeze duty on spirits, so that we can all afford to raise a wee dram to Ruth Davidson on the arrival of baby Finn, saving 2p on a pint of beer, 1p on a pint of cider and 30p on a bottle of Scotch or gin compared with the inflation assumption in the OBR (Office for Budget Responsibility) forecast, while proceeding with the usual RPI increases on wine.’
Reaction
Unsurprisingly, trade groups welcomed the outcome, whereas health experts were left disappointed by the lack of attention spent on dealing with the potential public health issues using fiscal means.
British Beer and Pub Association (BBPA) Chief Executive Brigid Simmonds said the beer duty freeze was ‘a big step in the right direction and a huge help for pubs across the UK that are struggling’, and that it will ‘save brewers, pubs and pub-goers £110m and secure upwards of 3,000 jobs that would have been lost had beer duty gone up.’ However, as James Morris of Alcohol Policy UK has pointed out, the BBPA’s claims about duty and the impact on jobs have been previously been contested by sections of the beer and pub industry in trade publications.
In contrast to the trade sector, alcohol policy modeller Colin Angus tweeted of the Budget announcement: ‘It’s certainly better than nothing, but it doesn’t seem likely to make any significant dent in the aims as set out when the measure was announced.’ He produced a ‘before and after’ graph of duty rates to illustrate the point.
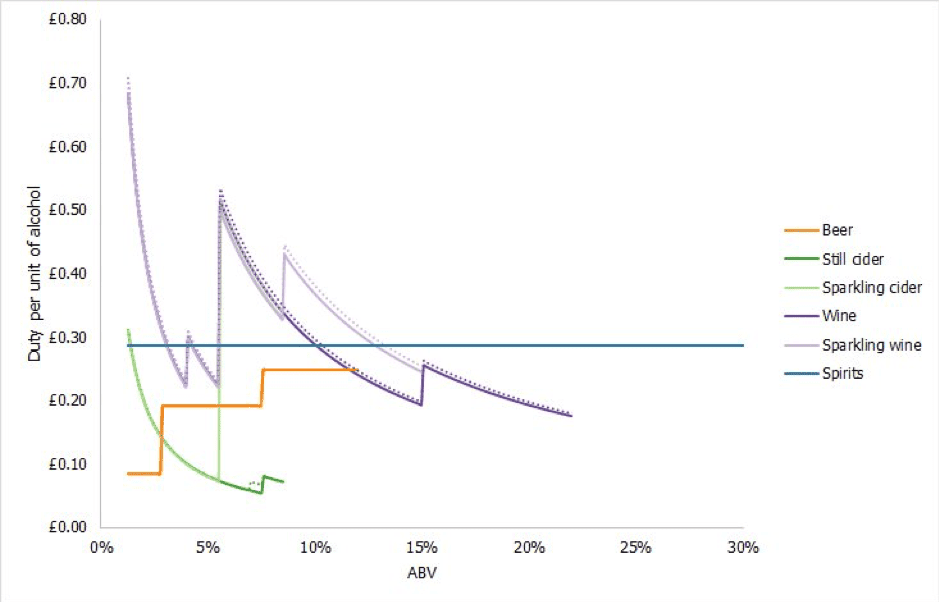
Alcohol duty rates, before and after. |
In the meantime, James Morris anticipates a continuation of the debate over alcohol duty rates in the run-up to Britain leaving the European Union in the spring of 2019, ‘with further scope for changes to alcohol duty structures’ after the 29 March 2019 deadline.
Alcohol Health Alliance Chair Professor Sir Ian Gilmore lamented the Budget as another ‘missed opportunity’ to demonstrate the government’s commitment to public health. He said:
‘The decision to freeze alcohol duty yet again represents a missed opportunity to take pressure off the NHS and other public services, and to protect the most vulnerable in our society.
‘In real terms, this freeze represents a cut in alcohol duty. Alcohol duty cuts since 2013 have already cost the Treasury about £4bn in lost revenue and will now cost another £5bn by 2023. At a time when our public services and specifically alcohol treatment services are under substantial pressure, we cannot afford any more duty cuts.
‘Alcohol is much more affordable today than it was 30 years ago, and alcohol-related harm continues to rise. With 65 people dying every day from alcohol-related causes, there’s an urgent need for government to take action on cheap alcohol.
‘Increasing alcohol duty is an effective and cost-effective measure to reduce alcohol harm and ease the pressure on the NHS, while raising additional revenue for public services at the same time.’
You can hear alcohol and drug charity Blenheim’s Chief Executive John Jolly talk about the Budget and how it impacts on his organisation’s alcohol policy aims in our Alcohol Alert podcast.
* 2016 prices
Liver disease still on the rise in England
Public Health England release data update
Public Health England (PHE) has updated its interactive liver disease profiles data tool with new hospital admissions figures.
According to local profiles data, in the financial year ending 31 March 2017, there were 68,364 admissions to hospital due to liver disease in England, a rate of 131.2 per 100,000 population, and the rate of hospital admissions from alcoholic liver disease was 38.5 per 100,000 population in England, a total of 20,202 admissions (illustrated, below).
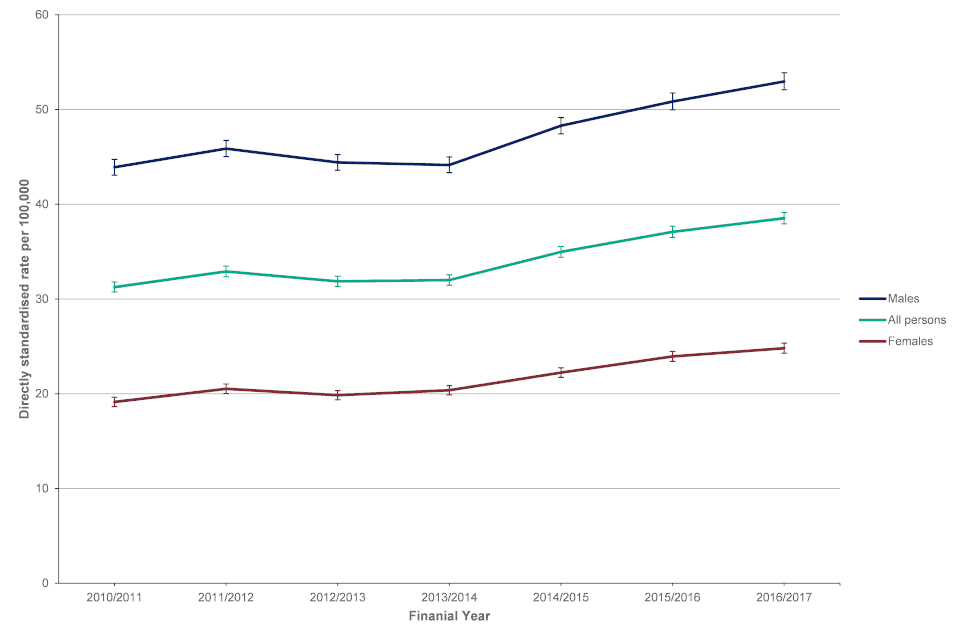 |
Both indicators have now been updated to 2016/17 and the time series fully revised back to 2010/11. The data show that the hospital admissions rates for liver disease patients have been on the rise for the last five years. In the case of alcoholic liver disease, the rate of hospital admissions for males is more than double that of females.
EU audiovisual law adopts light touch approach
MEPs decide to leave regulation up to Member States
02 October – There will no blanket European Union (EU) restrictions on alcohol adverts under the newly revised AudioVisual Media Services Directive (AVMSD), according to IEG Policy. Instead, individual Member States will be free to ban adverts for alcohol at their discretion.
MEPs approved the revision to the directive in a vote on 02 October. According to the European Commission webpage:
‘For alcohol advertising, the co-legislators agreed also to encourage further development of self- or co-regulation, if necessary also at EU level, to effectively reduce the exposure of minors to such advertisements. This does not prevent Member States from applying stricter rules such as, for example, banning alcohol advertisements or adopting other measures.’
Even a little daily tipple raises mortality risk
Light drinkers face 20% higher chance of premature death
03 October – Drinking a daily glass of wine for health reasons may not be so healthy after all, according to a new study from Washington University School of Medicine in St. Louis.
Analysing data from more than 400,000 people ages 18 to 85 in the journal Alcoholism: Clinical & Experimental Research, the researchers found that consuming one to two drinks four or more times per week – an amount deemed low risk by current guidelines – increases the risk of premature death by 20 percent, compared with drinking three times a week or less. The increased risk of death was consistent across age groups.
The Washington University study focused on two large groups of ‘light drinkers’ based in the United States: 340,668 participants, ages 18-85, in the National Health Interview Survey, and another 93,653 individuals, ages 40-60 who were treated as outpatients at Veterans Administration clinics. Light drinkers were defined as those who consumed only one or two drinks a day.
Although some earlier studies have linked light drinking to improvements in cardiovascular health, lead author Professor Sarah M. Hartz, MD, PhD, said that this study shows those potential gains are outweighed by other risks. Her team evaluated heart disease risk and cancer risk and found that although in some cases, drinking alcohol may reduce risk of heart-related problems, daily drinking increased cancer risk and, as a result, mortality risk. ‘Consuming one or two drinks about four days per week seemed to protect against cardiovascular disease, but drinking every day eliminated those benefits,’ she said. ‘With regard to cancer risk, any drinking at all was detrimental.’
‘It used to seem like having one or two drinks per day was no big deal, and there even have been some studies suggesting it can improve health,’ she added. ‘But now we know that even the lightest daily drinkers have an increased mortality risk.’
Speaking to Science Daily, Hartz predicted that as medicine becomes more personalised, some doctors may recommend that people with family histories of heart problems have a drink from time to time, but in families with a history of cancer, physicians may recommend abstinence.
‘If you tailor medical recommendations to an individual person, there may be situations under which you would think that occasional drinking potentially could be helpful,’ she said. ‘But overall, I do think people should no longer consider a glass of wine a day to somehow be healthy.’
Just the tonic, thanks: More young people shun alcohol
Study shows a drop in consumption, but reasons behind it remain unclear
09 October – Rising numbers of young people in England are becoming teetotal, and those who do consume alcohol are drinking less too, according to a new study published by researchers at University College London (UCL) in BMC Public Health.
Researchers at University College London analysed data on 9,699 people aged 16–24 years collected as part of the annual Health Survey for England, finding that the proportion of 16–24-year-olds who don’t drink alcohol has increased from 18% in 2005 to 29% in 2015.
The authors found a near doubling in the number of lifetime abstainers, from 9% in 2005 to 17% in 2015, to be a major contributory factor. There were also significant decreases in the number of young people who drank above recommended limits (from 43% to 28%) or who binge drank (27% to 18%). More young people were also engaging in weekly abstinence (from 35% to 50%).
Non-drinking ‘may becoming more mainstream’
Dr Linda Ng Fat, corresponding author of the study said: ‘Increases in non-drinking among young people were found across a broad range of groups, including those living in northern or southern regions of England, among the white population, those in full-time education, in employment and across all social classes and healthier groups.
Dr Fat also speculated that the widespread nature of the rise in abstinence suggests that it ‘may becoming more mainstream among young people’.
She went on to say: ‘The increase in young people who choose not to drink alcohol suggests that this behaviour maybe becoming more acceptable, whereas risky behaviours such as binge drinking may be becoming less normalised.’
Increases in non-drinking however were not found among ethnic minorities, those with poor mental health and smokers suggesting that the risky behaviours of smoking and alcohol continue to cluster.
What are these ‘New Puritans’ up to?
As it is an observational study, one cannot deduce clear-cut conclusions about cause and effect. However, the increasing long-term trend toward sobriety among young people has brought with it a great deal of speculation as to its the reasons why.
The title of the Telegraph’s coverage of the study ‘Millennials shunning alcohol as getting drunk is no longer cool’ strongly hinted at a classic generational divide between the activities of today’s young and their parents’ generation. The article referred to a 2017 survey by Eventbrite supporting this claim, which suggested that ‘millennials avoid getting drunk because they see it as something that old people do… only one in ten see getting drunk as “cool”… (whereas) they’re much more likely to consider it “pathetic” or “embarrassing”, with four in ten having an overall negative view of someone who is drunk.’
Dr Tony Rao of the Royal College of Psychiatrists also picked up on the theme. Speaking to the New Statesman, he said: ‘There’s less acceptance of drunkenness, behaviour that people used to see as culturally normal in the boomer generation… Young people [also] have a different way of social cohesion through social media, and they’ve also got better information about the harms from alcohol.’ Laura Willoughby MBE of the mindful drinking movement Club Soda still lamented the UK’s ‘alcohol-first culture’, where drinking underpins much of what constitutes adult social activity.
The phenomenon of declining youth drinking in the UK also caught the attention of the New York Times. The young people interviewed in its article Britain’s ‘New Puritans’: Youth Drinking Falls Dramatically suggested that ‘their peers had become more likely to resort to drugs like marijuana and ecstasy, which are often more accessible to minors than alcohol.’ However, surveys show that drug use, while still common, has also become less prevalent among young people.
Although the reasons behind the decline are unclear, Dr Fat concluded that ‘these trends are to be welcomed from a public health standpoint.’
‘Factors influencing the shift away from drinking should be capitalised on going forward to ensure that healthier drinking behaviours in young people continue to be encouraged’, she added.
Pregnancy warning labels mandatory for all alcohol
Adapted from SBS News
11 October – Alcoholic beverages must include a pregnancy warning label under a deal struck by the Australian and New Zealand governments, SBS News reports.
The alcohol industry has applied pregnancy warning labels on a voluntary basis since late 2011, and research has shown 74% of women aged 18–40 years are aware of the warnings on drink labels. But ministers responsible for food regulation who met in Adelaide say it needs to go further, amid evidence that babies exposed to alcohol in the womb can face intellectual, behavioural and developmental disabilities.
The label, which is to be developed by Food Standards Australia New Zealand in consultation with industry, will include a pictogram and warning statement.
Brewers Association Chief Brett Heffernan admitted that key players in the industry had recognised the current compliance rate under the voluntary system (75%) was not good enough.
‘Our members – Carlton & United Breweries, Lion Beer Australia and Coopers Brewery – have been 100% compliant with the voluntarily labelling regime since 2014, applying the warning pictogram across every product they produce,’ he said. ‘We are perplexed as to why others in the industry failed to heed the writing on the wall since 2012.’
The Brewers Association will seek to have the DrinkWise Australia warning become the standard.
French medics demand help to fund alcohol prevention
Adapted from The Local
12 October – A group of French doctors and medical professors have written to the country’s health minister Agnès Buzyn demanding an increase in taxes on alcohol to help fund an awareness campaign on the dangers of excess drinking.
The Local reports that the signatories of the letter lambasted the French Government’s current approach to preventing over-consumption as ‘ridiculous’.
Other requests to the letter include making provision for ‘a tax on alcoholic beverages’ proportional to the degree needed ‘to finance care’ for alcohol-related illnesses in the 2019 social security budget, as well as ‘a tax on advertising expenses’ to finance preventative measures.
Predictably, pro-industry figures came out against the move. In response to the letter, Alexis Capitant, representative of alcoholic drinks producers’ association Avec Moderation! told Franceinfo: ‘The problem with continually rising taxes is that it doesn’t help prevention, and it’s just lining the pockets of the state… it penalises consumers’ spending power, without any proven health benefits.’
The article states that alcohol taxes rake in €4 billion for the government annually, while alcohol-related illnesses end up costing France’s health system €120 billion every year. In health terms, alcohol consumption causes 49,000 annual deaths directly, and is the second biggest cause of cancer after smoking in France, the leading cause of death in 15 to 30-year-olds and the main cause of early onset dementia. Alcohol is also involved in more than half of all violence against women and children in the country.
Cross-party parliamentary group publishes its Alcohol Charter

Sir Ian Gilmore addresses audience |
Leading voices in alcohol recovery sector call on government to aim high with a new alcohol strategy
16 October – Thirty organisations across civil society have put their names behind a new Alcohol Charter urging the government to reduce the damage to society caused by alcohol.
The Alcohol Charter, published by the Drugs, Alcohol and Justice Cross Party Parliamentary Group and the All Party Parliamentary Group on Alcohol Harm, calls for the government to publish a new evidence-based alcohol strategy to improve support for those in need, protect public health and help tackle alcohol-related crime and disorder.
The document, prepared in consultation with the Alcohol Health Alliance, Alcohol Concern, Alcohol Research UK and the Institute of Alcohol Studies, entreats policy makers to follow the recommendations of the Public Health England alcohol evidence review and urgently tackle the increased availability of cheap alcohol and empower the public to make fully informed decisions about their drinking.
The Alcohol Charter calls on the government to outline concrete measures to moderate harmful drinking and address the million-plus alcohol-related hospital admissions each year in England. Without tangible counter measures alcohol is set to cost the NHS £17 billion in the next five years alone.
Drugs, Alcohol & Justice Cross-Party Parliamentary Group Co-Chair Mary Glindon MP said: ‘With dozens of alcohol-related deaths across the UK every day, we decided that rather than wait ages for the government’s Alcohol Strategy, we should promote a programme of actions which could reduce harm levels dramatically.’
Co-Chair Lord Ramsbotham said: ‘We believe action is needed urgently to address the cost to society inflicted by excessive alcohol. We hope our Charter will help focus attention on the issue; and that the government will adopt these concrete steps as a basis for their forthcoming Alcohol Strategy.’
Sir Ian Gilmore, Chair of the Alcohol Health Alliance, commented:
‘This Alcohol Charter is an important document which outlines many policies that the AHA has been calling for. The government needs to ensure that the upcoming Alcohol Strategy includes evidence-based policies which work to reduce alcohol harm and tackle the increased availability of super cheap alcohol. The best ways to do that is by introducing minimum unit pricing in England – which we already have in Scotland and will soon have in Wales – and increasing alcohol duty.’
Fiona Bruce MP, Chair of the All Party Parliamentary Group on Alcohol Harm, said: ‘With alcohol harm the leading cause of death among 15 to 49-year-olds, government must urgently take much stronger action to address this, and could do no better than by implementing the excellent proposals in our Alcohol Charter without delay.’
Ireland passes Public Health (Alcohol) Bill
Groundbreaking measure is first of its kind in Irish history
17 October – Legislation that includes provision for cancer warnings on alcoholic beverages and a minimum unit price for its sale is now on the Irish statute books, signed into law by President Michael D Higgins. Lawmakers passed the Public Health (Alcohol) Bill in both houses in the Oireachtas (national parliament) after three years of debate.
Ministers say the Bill, the first in Ireland to address alcohol as a public health issue, will help save lives. Addressing the Dáil, Health Minister Simon Harris said it was a ‘very special day’.
‘Alcohol damages our health, it harms our communities, it hurts many families and the measures in this Bill are designed to change that relationship,’ he said.
‘It’s about putting in place a number of measures for the first time ever in a public health perspective to try and change that corrosive culture that we currently have with alcohol in Ireland.’
Ireland is one of the top ten heaviest-drinking nations in the OECD in terms of quantity of alcohol consumed (illustrated), and ranks joint third for binge-drinking out of 194 countries, according to the World Health Organisation. The bill aims to tackle this problem by targeting:
- the affordable price of cheap, strong alcohol products (with a minimum price per unit of alcohol),
- the marketing and promotion of alcohol to children and young adults,
- the intrusive availability and visibility of alcohol products in small shops, convenience stores and supermarkets, and
- the presence on all alcohol products, and its promotion, of adequate health information (eg warnings of the link between cancer and alcohol, the number of calories, etc), so that citizens can be accurately informed of the risks of consumption.
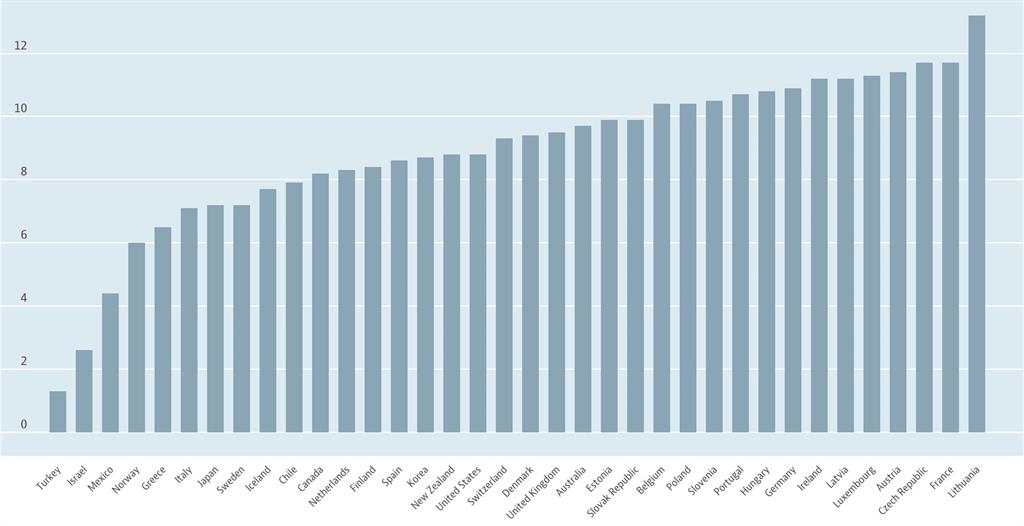
Irish consumption levels are seventh highest of OECD nations. |
Commenting on the outcome, Suzanne Costello, CEO, Alcohol Action Ireland, said:
‘Today’s success has been slow in the making but its testimony will stand as credit to those people who have contributed their time and energy, many on the whole voluntarily, to bring about this innovative and progressive piece of public health legislation.
‘The Bill will not be a panacea to all our entrenched societal difficulties with alcohol. However, it is a very significant start and over time, perhaps a generation – just as we did with tobacco – with sustained leadership, we can begin the forge a new relationship with alcohol, one that appreciates the potency and risk to both our mental and physical wellbeing.
‘Over 3,000 people have died from alcohol related illness and incident in the period that this legislation was before the Oireachtas; that’s three people yesterday, and today but our tomorrows can be better.’
Majority support higher alcohol taxes to fund public services
Adapted from Alcohol Health Alliance UK website
24 October – New figures reveal that just over half (52%) of people support increasing alcohol taxes if the money raised went into funding public services impacted by alcohol use, such as the NHS and police. The survey also showed that less than a fifth (19%) of people would oppose such a measure.
The recent online survey, conducted by the Alcohol Health Alliance UK, comes as leading voices in the alcohol recovery and public health sector are calling on the government to increase alcohol duty by 2% above inflation ahead of the Autumn Budget.
With the promise of an additional £20 billion for the NHS, the government needs to find new streams of revenue. Reports over the summer suggested that the government was considering increases to alcohol and fuel duty to help pay for this. However, following significant pressure to abandon these proposals, Prime Minister Theresa May announced earlier this month that fuel duty would remain frozen; making it even more urgent to find a way to finance the commitment to the NHS.
The new polling indicates that the government would have the support of the public to press ahead with an increase in alcohol duty to help fund the NHS. While such a move would increase the revenue for the Treasury, it would have the double effect of also reducing demand and costs on the NHS.
Alcohol puts considerable pressure on the NHS with more than a million alcohol-related hospital admissions and thousands of alcohol-related deaths every year. Increasing alcohol duty above inflation for five successive years would prevent more than 600 alcohol-related deaths every year.
Successive cuts in alcohol duty since 2013 have cost the government £4 billion in lost revenue – equivalent to the salaries of almost 40,000 GPs or more than 120,000 social workers.
Sir Ian Gilmore, chair of the Alcohol Health Alliance, said: ‘With our public services overstretched already, we can’t afford for alcohol to get any cheaper. Increasing alcohol duty will help to curb the pressure on the NHS, while creating additional revenue for the government. This survey shows that the majority of the public support an increase in alcohol duty if the money raised is spent on services impacted by alcohol use, such as the NHS.’
A separate survey carried out in the North East of England recently showed that publicans see no benefit to their businesses from alcohol duty cuts and that they need measures which help them compete with supermarkets.
Landlord Ian McNaughton, of The Falcon Inn in North Yorkshire, believes cheap supermarket alcohol is a cause for the closure of pubs, especially in rural areas.
He said: ‘I think that cuts in alcohol duty only benefit supermarkets. We are led to believe that this is a measure that helps pubs and landlords such as myself, but it is putting us at a greater disadvantage and enabling supermarkets to capitalise on cheaper alcohol to attract customers and drive their profit.’
Pre-watershed moment for alcohol ads ‘common’
Kids regularly see alcohol promoted on TV before 9PM
25 October – A Journal of Public Health study indicates that the common occurrence of alcohol advertising on British television may be a potential driver of alcohol use in young people.
An estimated 28 million British households have at least one television and in 2015 the average viewing was 3 hours and 47 minutes a day. Previous studies have found that alcohol imagery appeared frequently in studies of UK television; some 40% of programs contained alcohol content.
In 2015, researchers quantified the content of all programs and advertisements broadcast on the five, free access, national UK channels. The researchers here explored the differences in content between channels and genres, and compared these with the findings of a similar study in 2010.
A total of 611 programs and 1,140 commercials were recorded during the peak viewing hours, between 6 and 10PM, from Monday to Sunday in three separate weeks. Alcohol imagery occurred most frequently in the news, current affairs programs, and soap operas.
This study demonstrates that alcohol imagery is extremely common on UK television, occurring in over 50% of all programs broadcast and almost 50% of all advertising periods between programs. The majority of alcohol content occurred before 9PM, otherwise known as ‘the watershed’, when content deemed unsuitable for children can be broadcast. Branding occurred in 18% of programs and 11% of advertisement periods and involved 122 brands, though three brands (Heineken, Corona, and Fosters) accounted for almost half of all brand appearances.
The analysis shows that television remains a major source of alcohol exposure to young people in the UK and is likely to continue to be a contributor to alcohol uptake by young people, with levels of content slightly higher than the researchers observed in the earlier analysis of program content from 2010.
‘There is strong evidence that viewing alcohol advertising or imagery has an uptake on subsequent alcohol use in young people,’ said Alexander Barker, research fellow at the Centre for Tobacco and Alcohol Studies. ‘Our study shows that alcohol imagery, including branding, is regularly broadcast on prime-time TV, when children and adolescents are likely to be watching.
‘Tighter scheduling rules from the Advertising Standards Agency and Ofcom (broadcast regulator), such as restricting alcohol advertisements and alcohol imagery in programs, to after the 9PM watershed, could prevent children and adolescents being exposed to this content.’
Alcohol industry CSR may do more harm than good
Content analysis finds its effectiveness is illusory
26 October – Alcohol industry corporate social responsibility (CSR) schemes strengthen their own commercial interests while failing to meaningfully reduce harmful alcohol use, according to a new report published in the BMJ Open.
The study of industry CSR actions across six global regions found that almost all of them (96.8%) lacked scientific support. Meanwhile, alcohol producers benefitted from brand exposure and the appearance of being able to manage risk and achieve strategic goals.
The research team employed a content rating procedure to analyse 30% (N = 1,046) of 3,551 industry-sponsored actions described in an online database website maintained by the International Alliance for Responsible Drinking (IARD).
Actions were assessed on the basis of their global distribution according to United Nations regions, the benefits reaped to the industry in terms of marketing potential, impact on regulatory policy, and type of CSR strategy, and the public health impact of the industry actions were evaluated in terms of their likely effectiveness and potential harm.
The industry actions were found to have been conducted disproportionately in regions with high-income countries (Europe and North America), compared with lower proportions in Latin America, Africa and Asia.
In addition to a widespread lack of scientific rigour behind the actions, only a quarter (27%) conformed to the recommended World Health Organisation (WHO) target areas for global action to reduce the harmful use of alcohol, and 11% had the potential for doing harm.
Commenting on the report, lead author Professor Thomas Babor, head of the Department of Community Medicine and Health Care at the University of Connecticut said of the findings:
‘The corporate social responsibility activities of alcohol producers conceal a clear conflict of interest in improving public health, as a truly effective approach to tackling alcohol harm will only hurt their bottom line. Governments, however, have a clear duty to put public health first and must do so without industry interference.’
Katherine Severi (née Brown), chief executive of the Institute of Alcohol Studies and one of the report authors, said:
‘This paper shows there is sufficient evidence to believe that the alcohol industry’s claims to be a responsible actor in reducing harms are illusory, and in fact may be actively detrimental to people’s health across the globe.
‘With rates of death and disease on the increase in the UK, we cannot afford to delay meaningful action, and that can only come from the government looking at the evidence of what works. Data from home and abroad is crystal clear, tackling the availability of ultra-cheap alcohol through tax increases and minimum unit pricing will bring huge improvements to the health of the nation.’
SHAAP report examines Scottish alcohol mortality
Dying for a drink report |
Group calls for ‘professional optimism’ to support recovery from alcohol problems
26 October – The new SHAAP (Scottish Health Action on Alcohol Problems) report Dying for a drink shines a light on the nature of alcohol mortality in Scotland, drawing on interviews with those affected to highlight the personal tragedies caused by harmful alcohol use.
The group also calls for more ‘professional optimism’, both to recognise that people can recover from alcohol problems and to support that process. The new SHAAP report draws attention to the fact that alcohol-related deaths remain significantly higher in Scotland than in England and Wales where death rates are high by international standards. It also points out that although there has been a downward trend in deaths since the mid-2000s, this may now have levelled off. The two main causes of alcohol-related deaths in 2017 were alcohol-related liver disease (738 deaths, 60%) and mental and behavioural disorders caused by alcohol (321 deaths, 22%). There were a total of 1,235 deaths in 2017. Alcohol-attributable deaths (AADs) include an appropriate proportion of a further 30 causes of death which are partially caused by alcohol. Using this wider definition, there were an estimated 3,705 deaths attributable to alcohol in Scotland in 2015.
The new SHAAP report also indicates that different sections of the population are harmed by alcohol in a range of different ways: The main causes of AADs for people under 35 are suicide, road/pedestrian accidents and poisoning. The main causes of AADs for people over 35 are alcohol-related liver disease, mental and behavioural disorders and neoplasms of the breast and oesophagus.
SHAAP notes that men are approximately twice as likely to have an alcohol-related death as women – this has remained constant over time. The impact of poverty is also highlighted: people living in the 10% most deprived areas are at least six times more likely to die because of alcohol use than those living in the 10% least deprived areas.
Interviews conducted with individuals regularly engaged in excessive drinking, those in recovery, family members and professionals working in this area, found that:
- Alcohol-related problems are symptomatic of many deep-seated and personal issues. The main reasons given by those continuing to drink and those in recovery were addiction taking hold; to gain confidence; deal with abuse as child; adult trauma; self-hatred; mental health issues and no longer caring for oneself
- User voices are both invaluable and necessary, and those with lived experience have to be a part of the conversation around strategy and service development
- The steps towards recovery and sustaining recovery are about relationships and not doing this alone but with the support of others. Importantly, all people, at all levels in society, including though not limited to professionals, can play a powerful role in challenging stigma, showing care to help build hope, and demonstrating in daily actions the value of compassion and humanity
- Alcohol harms are complex, affecting individuals and people around them. This research brings to light the shame and stigma families feel about dealing with this issue, the variability of service provision, and in some cases a lack of compassion and understanding they face, both by ‘society’ and professionals
- Inequalities and a ‘Scottish drinking culture’ play major parts in contributing to alcohol-related deaths, according to professionals
- Alcohol issues need to be addressed within a public health paradigm, i.e. at individual, social and societal levels
- Resources invested ‘upstream’ in prevention will save money, and more importantly, lives in future.
Dr Eric Carlin, Director of SHAAP, who led the study said:
‘The people we spoke to in this study told us that that we need to establish a continuous dialogue with those affected by alcohol problems, including drinkers and their families, to understand what social and health harms they experience. Their insights should inform strategies to prevent and reduce alcohol-related harms and early preventable deaths.
‘“Professional optimism” in all public services should promote the idea that people can, and do, recover from alcohol-related problems, with support from their communities. All public services, including housing, welfare and employment services, should be alerted to the potential risks of harmful drinking, so that triggers for intervention are understood and support is embedded in service delivery. Working in collaboration, all public services, including housing, welfare and employment services, should be alerted to the impact of psychological problems, trauma and bereavement, on harmful drinking, as part of key training for all staff who have contact with the public.
‘We also need to challenge stigma related to people who use alcohol harmfully, as it adds to the barriers that people face in accessing services. The potential contribution of assertive outreach services to supporting engagement in services should also be considered.
‘Prevention also remains important. SHAAP has long been at the forefront of campaigning for policies to reduce and prevent alcohol harm from happening in the first place. The findings from this review underline the importance of continued support for policies to increase price, reduce availability and marketing in order to be effective in reducing overall population consumption and harms.’
Number of 24-hour licensed premises creeps up
Abridged from Alcohol Policy UK
Off-sales only premises licences exceed that |
26 October – The Home Office have released 2018 statistics on alcohol and late night refreshment licensing in England and Wales, showing a further small but consistent rise in the total number of licensed premises. The release also includes a short consultation on the statistical bulletin.
As seen in recent years, a further small rise of 1,100 (1%) in the total number of licensed premises (212,800) has been recorded since last year. In addition to total premises licenses, figures also show in March 2018 there were:
- 723,800 personal licences, a 5% increase (35,600)
- 14,100 club premises certificates, a 1% decrease (200)
- 8,100 premises with 24-hour alcohol licences, a 6% increase
- 222 cumulative impact areas in place
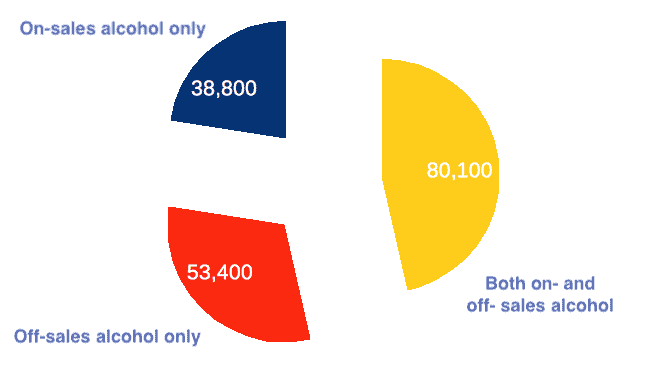
172,300 premises licences in England and Wales were permitted to sell alcohol, of which 23% were for on-sales of alcohol only (38,800 licences), 31% were for off-sales of alcohol only (53,400 licences), and 46% were for both on- and off- sales (80,100 licences) (illustrated, top right).
Cumulative Impact Policies (CIPS) are available for local authorities (LAs) to designate ‘saturation zones’ in a bid to curb further premises from opening where it is deemed likely to increase problems. The latest bulletin reports 107 LAs had a total of 222 CIAs in place in 2015, suggesting just one new CIP in the last year. Previously there have been highlighted issues over reported CIP data questioning its accuracy and what effect they were having in practice, although a study published last year found areas which had higher use of CIPs were associated with decreased alcohol-related crime rates in the period up of 2009 to 2013.
 |
The Late Night Levy (LNL) began to be adopted in 2013, allowing LAs to raise a contribution from late-opening alcohol suppliers towards policing the night-time economy. Late night levies must cover the entire LA area and apply for a specified period between 12am and 6am. The latest figures show no change in the eight LAs with LNLs in place, with revenue down slightly from £1.8 to £1.7 million this year. No Early Morning Restriction Orders (EMROs) have been implemented. In 2012 the Association of Licensed Multiple Retailers announced a ‘fighting fund’ to support legal challenges against EMRO and LNL plans.
 |
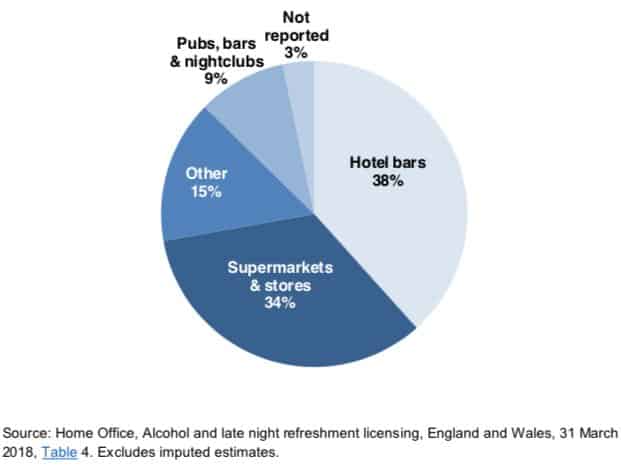
There were 8,100 premises with 24-hour alcohol licences as at 31 March 2018, a 6% increase on the previous year. The majority apply to hotel bars and supermarkets (illustrated, left). Temporary Event Notices (TENs) authorise one-off events involving licensable activities, with 147,200 TENs in the last year; a 6% increase (8,900) compared with the previous year.
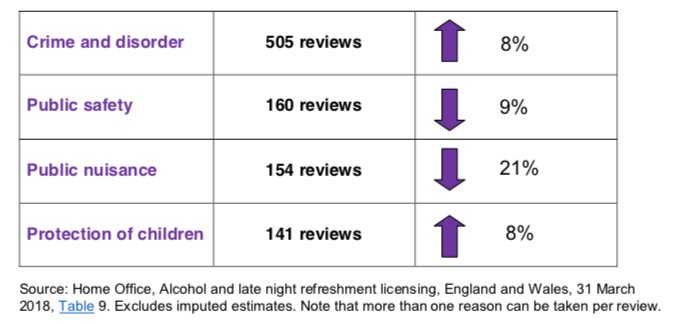
The Home Office release also reveals that local authorities conducted just over 600 reviews of licences as at 31 March 2018. Despite this being a slight increase on the previous year, this continues the long term decline since 2010, when approximately 1,300 were carried out, (illustrated, right).
For the full story, please visit Alcohol Policy UK.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads

