In this month’s alert
Editorial – September 2020
Hello and welcome to the Alcohol Alert, brought to you by The Institute of Alcohol Studies.
In this edition:
- A round-up of how alcohol drinkers, producers and retailers have fared as the prospect of a second coronavirus wave looms
- Think tank finds NoLo drinks have limited impact 🎵 Podcast feature 🎵
- SHAAP and IAS launch the Men and Alcohol report
- Numbers of alcohol-related admissions to English hospitals continue to rise
- Poll shows almost half of Scots surveyed now back minimum pricing for alcohol
- Backlash over NICE plans to record pregnant womens’ consumption
- We announce the winners of our Small Grants Scheme
We hope you enjoy our roundup of stories below: please feel free to share. Thank you.
Drinking in the second wave of a pandemic
Coping with COVID-19: Alcohol offers little comfort to solitary drinkers
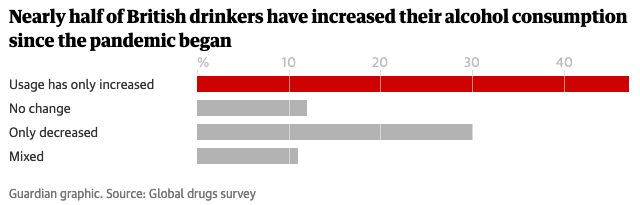
One of the enduring stories of 2020 has been the question of how some people use alcohol to cope with new ways of living in the time of COVID-19. One of the many research attempts to find this out, the Global Drug Survey (GDS), found that almost half (48%) of Brits have so far upped their alcohol intake during the pandemic, ‘due to loneliness, depression and anxiety’ (Guardian, 09 Sep).
Furthermore, 30% of drinkers said increased alcohol consumption had worsened their mental health and 47% disclosed that their physical health had deteriorated.
Researchers found that increased use of both alcohol and cannabis due to anxiety, loneliness or depression was significantly higher among people with a pre-existing mental health or neurodevelopmental condition. That group of respondents were at least twice as likely to report worse mental health (38%) due to drinking more alcohol than those without such conditions (19%).
The study also highlighted the limitations of a substance perceived as having some social purpose: when the venue for consuming alcohol is removed from people’s lives, drinking for some doesn’t simply stop, but instead manifests in other potentially unhealthy ways. The number of people drinking alone at home while on audio or video calls, such as Zoom meetings, or during ‘watch parties’, where friends view and discuss films and TV programmes together via group chat, increased from 17% to 38%.
Comparing alcohol with cannabis, professor Adam Winstock, GDS chief executive, observed: ‘People’s drug use is hugely dependent upon being able to socialise and when that ability goes away, people turn to drugs that they’re already familiar with – cannabis and alcohol. But the impact of increases of those two drugs is quite distinct, and those drinking more alcohol come off worse.’
Closing time for COVID? Pubs on curfew
Some spending data indicated the desire on the part of some to resume pre-pandemic habits, but the results were mixed, ‘with like-for-like [August] sales down 3·6%’ against the same month last year (This is Money, 28 Sep).
Signs of economic recovery were likely the focus of discussions between Hospitality Ulster and Stormont ministers about the prospect of reopening drink-only pubs (BBC News Northern Ireland, 07 Sep).
But with an uptick in the number of coronavirus cases in September, attention turned to whether and how pubs – the symbol of a nation trying to return to some kind of normal – were keeping customers safe (BBC News Business, 13 Sep)?
In England, hospitality businesses (including pubs) became legally mandated to take customers’ contact details so they can be traced if a potential outbreak is linked to the venue. These rules were in addition to the new ‘Rule of Six’, which limits the number of people allowed to meet each other.
Some pubs experienced small outbreaks within their own workforce: the JD Wetherspoon chain reported 60 Wetherspoon staff across 50 branches had tested positive for COVID-19 (Mirror, 14 Sep).
Meanwhile, rumours spread of the possibility of implementing curfews on pub opening hours if the number of new coronavirus cases did not fall over the next few weeks (Daily Star, 14 Sep). A survey of more than 4,000 UK adults found that 69% would be favour of a 9PM curfew (YouGov, 15 Sep).
And so, the government made plans to shut the pubs… at 10PM (BBC News, 22 Sep). While BBC health correspondent Nick Triggle wondered whether the move would be of marginal benefit in staving off the threat of the virus, chair of the Public Accounts Committee Meg Hillier asked the prime minister how the government was able to square their proposal with extending alcohol licensing provisions for pubs to acquire pavement licences for eating and drinking on the public highway?
22/09/2020: @CommonsPAC chair Meg Hillier asks the prime minister the rationale behind the 10 o'clock curfew for pubs weeks after permitting licensed venues to sell alcohol for consumption off the premises pic.twitter.com/TiOLJkyxie
— IAS (@InstAlcStud) September 24, 2020
For all the government’s desire to strike a balance, representatives of the hospitality industry still claim that a curfew will neither help curb the virus nor the commercial viability of their businesses, which are ‘still on life support’. Talking to trade outlet Morning Advertiser (22 Sep), Fuller’s chief executive Simon Emeny called pubs ‘the home of responsible socialising’ and said his company had worked hard to implement safety measures across its pubs, to be rewarded with unnecessary restrictions, while Peter Borg-Neal, chief executive at multiple operator Oakman Inns, said he saw little public health benefit but ‘lots of economic damage’ instead.
Can addiction treatment services survive a second wave?
Whatever happens in the coming weeks, it is clear that our addiction services can ill afford to combat the swelling number of high risk drinkers seeking treatment alongside a second wave of COVID-19 cases. Royal College of Psychiatrists analysis of Public Health England’s latest data on the indirect effects of COVID-19 found that over 8·4 million people are now drinking at higher risk, up from just 4·8 million in February. But the multi-million-pound cuts made to addiction services since 2013/14 mean they could miss out on life-saving treatment (14 Sep).
Professor Julia Sinclair, chair of the college’s addictions faculty, said: ‘COVID-19 has shown just how stretched, under-resourced and ill-equipped addiction services are to treat the growing numbers of vulnerable people living with this complex illness.
Drug-related deaths and alcohol-related hospital admissions were already at all-time highs before COVID-19. I fear that unless the government acts quickly we will see these numbers rise exponentially.’
Think tank: NoLo drinks have limited impact
🎵 Podcast feature 🎵
A report on no and low alcohol beverages (‘NoLo’) from the Social Market Foundation finds limited evidence for their impact on health outcomes (08 Sep). Sponsored by Alcohol Change UK (ACUK), the publication finds that whilst NoLo products may help individuals reduce their consumption, they are unlikely to produce the aggregate level reductions in alcohol-related harms public health experts would desire.
The key findings were:
- The market for NoLo drinks – whilst brands continue to release new products into the NoLo drinks category – worth around £110 million in 2018/19 – it is thought NoLo products comprised just 0·2% of the total market for alcoholic drinks in that year. The report estimates that annual sales growth of NoLo drinks would have to exceed over 40% per annum for market share to stand above 10% by 2030
- Consumers in the NoLo market – survey results commissioned specially for this study found that one in five people (21%) have consumed an alcohol-free beer, cider, wine or spirit in the last year. Including low-strength drinks (up to 1·2% alcohol content), this rises to 27%. Young people and those in higher income socioeconomic groups were more likely to have tried a NoLo product
- The regulation of the NoLo market – Guidance and ABV descriptors issued by the Department of Health and Social Care contains elements of ambiguity and are often out of step with other European countries
- The presentation of NoLo products – press coverage of NoLo drinks typically centres on the ‘new sensibility’ of younger people and NoLo as a ‘community’ or ‘movement’. Some producers have tapped into this by promoting their NoLo products as substitutes for stronger products. Others prefer to market them as additional to existing drinks on the market
- The impact on alcohol-related harms – survey results for this report indicate that among those that have consumed NoLo drinks over the past 12 months, about four in ten have cut back on their alcohol consumption. However, a similar number reported no change. A significant proportion of consumers of NoLo also indicated that they do so on top of, rather than instead of, stronger products. This raises concerns about how NoLo products can tackle alcohol-related harms at the population level
- Considerations for policy – whilst the Government has indicated that NoLo products will be key to reducing alcohol-related harm, this report cautions that NoLo drinks must form part of a much wider harm prevention strategy. Government should also consider reforming ABV descriptors for NoLo and legislate to protect against alibi marketing.
Commenting on the findings, ACUK director of research and policy Lucy Holmes said (you can listen to our interview on NoLo drinks in our podcast):
MPs and peers call on government to urgently address Britain’s alcohol harm crisis
Abridged from the Alcohol Health Alliance UK press release
As the leading risk-factor for ill health, death and disability among those aged 15 to 49 in England, alcohol is inflicting long-lasting harm across all areas of society and family life, yet not enough is being done to tackle the problem, say a group of cross-party parliamentarians, who are calling on the government to develop an alcohol strategy to get to the heart of the nation’s drink problem.
Under the independent Commission on Alcohol Harm was set up by alcohol health experts and parliamentarians to examine the full extent of alcohol harm across the UK.
Evidence submitted to the Commission highlights the serious impact alcohol harm has on family life, with children living with an alcohol dependent parent five times more likely to develop eating disorders, twice as likely to develop alcohol dependence or addiction, and three times as likely to consider suicide. The accompanying online launch also saw moving testimony from those whose lives have been harmed by alcohol.
The Commission concluded that a new UK-wide alcohol strategy is required urgently. Recommendations from the final report include (summary):
- The new alcohol strategy must include targeted measures to support families and protect children from harm, including alcohol-fuelled violence
- The new alcohol strategy must be science-led and adopt the World Health Organization’s evidence-based recommendations for reducing the harmful use of alcohol. This includes measures on affordability – such as the introduction of minimum unit pricing in England – and restrictions on alcohol advertising and marketing – such as ending sports sponsorship, better information for consumers, advice and treatment for people drinking at hazardous and harmful levels, and action to reduce drink-driving
- Reducing the £3·5bn cost of alcohol to the NHS would help to relieve pressure on the service and free up capacity to respond to the consequences of COVID-19
- Changing the conversation and challenging alcohol’s position in our culture. This means addressing the stigma around alcohol use disorders, encouraging conversations about drinking to take place more easily and creating space for people to be open about the effects of alcohol on their health and those around them.
Professor Sir Ian Gilmore, chair of the Alcohol Health Alliance said (you can also hear his thoughts on the report in the podcast): ‘When people think about alcohol harm, they often think about liver damage – but its impact goes much further than this. This report highlights the very real ways that alcohol can devastate not just the life of the drinker but those around them. If we wish to emerge from the coronavirus pandemic as a healthier society, we must address the ongoing health crisis of alcohol harm.’
If you want to help the Alcohol Health Alliance reach decision makers so they take action to reduce alcohol harm, you can – follow the link below to share the report with your local MP.
Launch of Men and Alcohol report
Scottish Health Action on Alcohol Problems (SHAAP) and the Institute of Alcohol Studies (IAS) have launched a new report presenting key findings and recommendations for policy and practice from their 2019/2020 Men and Alcohol seminar series (09 Sep), along with a webinar discussion of key themes raised.
The report highlights how alcohol consumption is closely connected to male identity, and that alcohol-related harms, both mental and physical, remain a significant issue for men in the UK, with men less likely to seek help for mental health problems.
Key recommendations for policy include: calls to strengthen restrictions on alcohol availability; to enforce bans on alcohol advertising, sponsorship and promotion; to make alcohol less affordable via taxation and pricing policies, and to invest in youth services and ‘alcohol-free’ spaces to help prevent alcohol-related harm.
The report’s recommendations for practice address the need for all services to be joined-up, trauma-informed and exercising professional optimism, and emphasise that services should be guided by the expertise of individuals with lived experience in order to reduce the stigma of seeking help.
Alcohol-related admissions to hospitals rising
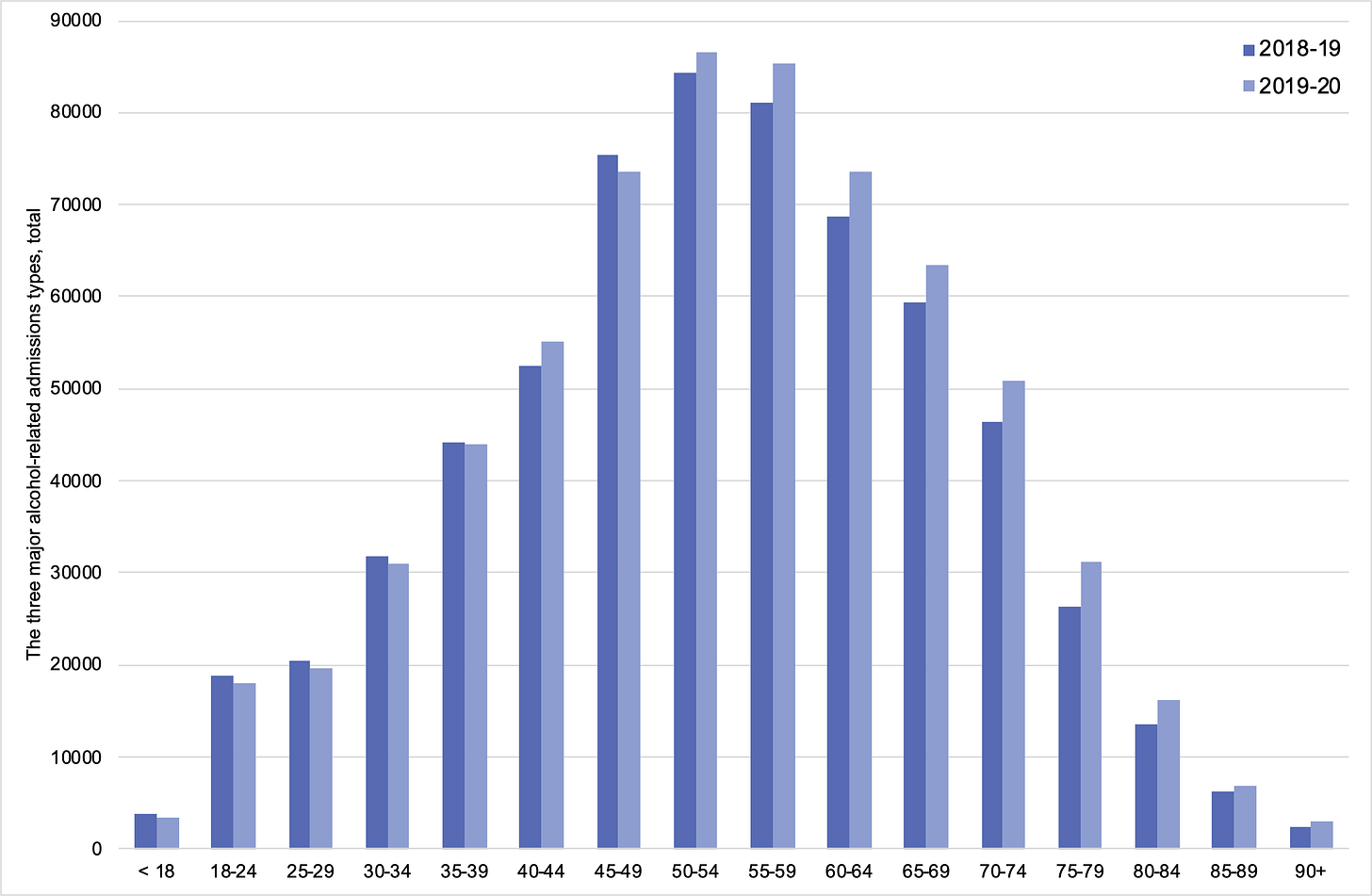
NHS Digital’s latest release on patient care activity in English NHS hospitals (17 Sep) has found that there were nearly 670,000 admissions by diagnosis for the three most common alcohol-related case types (Mental and behavioural disorders due to use of alcohol, Alcoholic liver disease, and Toxic effects of alcohol) in 2019/20.
The number of admissions marks a 4% increase on the previous year: there were approximately 644,000 admissions in 2018/19. As the main diagnosis, the three main case types totalled just over 120,000 admissions, 2% up on the previous period, when there were almost 118,000.
When split by case type, the majority (69%) of the three major alcohol-related admissions were for Mental and behavioural disorders due to use of alcohol (459,468), of which it was the main diagnoses for 68,128 admissions. A quarter were for Alcoholic liver disease (170,031), of which it was the main reason for 50,561 admissions. 6% were for the Toxic effects of alcohol (40,337), of which it was the main reason for 1,329 admissions.
The majority of cases were male (67%), and when split by age, those in their fifties were most frequently admitted to English hospitals in 2019/20. There were across-the-board increases in admissions for patients aged 50 years and above compared with 2018/19.
In other research
Almost half of Scots surveyed now back minimum pricing for alcohol: 49·8% of 1,022 people surveyed by Public Health Scotland supported the measure (22 Sep).
https://twitter.com/MESAS_phs/status/1308348146850951169?s=20
The survey comes as research published in Health Economics finds that minimum unit pricing (MUP) has had a successful initial impact on increasing alcohol prices (thus reducing affordability) and reducing alcohol sales (and consumption by proxy). The paper found that the impact of MUP on alcohol prices and sales is most pronounced on off‐premise venues (15 Sep).
And in Wales, polling commissioned by Alcohol Change UK Cymru found that three quarters of 1,000 respondents knew about MUP compared with just half of drinkers in Wales when asked a year ago, and that of those who were aware of its implementation six months ago, 10% were drinking less alcohol because of it (Bro Radio, 28 Sep).
Using publicly available national data (including Hospital Episode Statistics), a study conducted by the University of Hull reported that a decrease in admissions to specialist alcohol inpatient services subsequently marked an increase in admissions to acute hospital services (Alcohol and Alcoholism, 04 Sep). This decrease in admissions to specialist treatment centres has been associated with significant reductions in public health funding to such services since the introduction of the Health and Social Care Act 2012. However, these reductions have resulted in a shift of service use, particularly placing increasing pressures on emergency departments due to a larger number of patients with chronic alcohol disorders accessing care.
A new paper conducted by the London School of Hygiene and Tropical Medicine, Dark Nudges and Sludge in Big Alcohol: Behavioral Economics, Cognitive Biases, and Alcohol Industry Corporate Social Responsibility, evaluates the roles of dark nudges and sludges in the alcohol industry (Milbank Quarterly, 15 Sep; video summary here). It shows how alcohol industry bodies such as Drinkaware use dark nudges and sludges to influence consumers’ views, often against their best interests. In particular, messages promoting the ‘social norms’ of drinking are frequently distributed, for example the technique of ‘omission biases’ in the infographic ‘Alcohol and the body’ from Drinkaware Ireland, which, by omitting women, consequently fails to highlight that breast cancer is also a major hazard of alcohol consumption.
A multicohort study conducted by University College London has shown that those who have reported losing consciousness due to alcohol consumption (regardless of their weekly intake) have double the risk of developing dementia, compared with moderate drinkers who never lost consciousness (JAMA Network, 09 Sep). Overall, those who were moderate-to-heavy drinkers had a 1·2-fold greater risk of developing dementia in the long-term. Alcohol misuse was seen to cause brain atrophy and neuronal loss in several areas of the brain, such as the frontal cortex. Other side-effects of heavy drinking, such as hypertension, can also be attributed to dementia.
Plans to record pregnant womens’ consumption not so NICE
Pregnancy rights’ advocates have criticised a proposal from National Institute for Health and Care Excellence (NICE) of a Quality Standard to record pregnant women’s alcohol consumption on their child’s medical records in England (Guardian, 16 Sep).
NICE’s proposal was drawn up as part of a consultation to cement guidelines for doctors to diagnose and prevent foetal alcohol spectrum disorder (FASD). Proponents argue that the risk of FASD – a range of physical and mental conditions caused by drinking in pregnancy – to an unborn child should be the reason for prioritising their needs.
However, pregnancy charities including the British Pregnancy Advisory Service (BASP) and Birthrights suggested that the guideline on recording alcohol consumption could be a breach of the expectant mother’s confidentiality, and therefore fall foul of data protection regulations.
A quarter of adopted UK children may have symptoms of FASD
The results of an Adoption UK survey of nearly 5,000 adopters underscore FASD campaigners’ concern about drinking habits during pregnancy: one in four adopted children are either diagnosed with or suspected to have a range of conditions caused by drinking in pregnancy (Guardian, 29 Sep).
8% of children had a diagnosis, and a further 17% were suspected by their parents to have foetal alcohol spectrum disorder (FASD),
The survey also showed 55% of families polled had waited two years or longer for an FASD diagnosis, and 78% felt healthcare professionals lacked basic knowledge about the condition.
Maria Catterick, director of the FASD Network UK, said the statistics were unsurprising given that ‘alcohol, drugs and domestic abuse are major reasons why children are placed into the care system’.
Small Grants Scheme awards announced!
We are delighted to announce that we will be funding three projects led by early career researchers in the alcohol field through the new IAS Small Grants Scheme.
Proposals were considered in a two-stage process and reviewed externally. This was a highly competitive round and the standard of applications overall was extremely high. Feedback was provided to all applicants. We will be funding the following projects in the coming months:
- Dr Elena Dimova, Glasgow Caledonian University: Exploring men’s alcohol consumption in the context of becoming a father: A scoping review
- Jessica Muirhead, Wrexham Glyndŵr University: Effective online age gating using MCC codes
- Dr Emily Nicholls, University of Portsmouth: Rewriting the rules or playing the game? An investigation into the ways in which social norms around gender & drinking are challenged &/or reinforced through the promotion, marketing & consumption of Alcohol-Free drinks
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads