View this report
Summary
- Health inequalities are usually defined as systematic differences in health outcomes between socioeconomic groups
- Alcohol has been implicated as both a determinant and an outcome of socioeconomic inequality
- The ‘alcohol harm paradox’ is the name given to the phenomenon where there is greater alcohol-attributable morbidity and mortality among the most deprived socioeconomic groups compared to the least deprived groups, despite similar levels of alcohol consumption
- Researchers have linked alcohol consumption with socioeconomic inequalities – reducing the availability of alcohol would ‘reduce adverse health outcomes among lower socioeconomic groups’
Introduction
Health inequalities are usually defined as systematic differences in health outcomes between socioeconomic groups, categorised by indicators such as household income, educational qualifications, housing tenure and area deprivation. Importantly, health inequalities also exist between groups identified using other social constructs such as race, ethnicity and gender.
There is a substantial evidence base identifying links between alcohol and health inequalities. Those in the most socioeconomically deprived decile have 2.23 times the rate of alcohol-specific mortality and 1.53 times the rate of alcohol-related mortality compared to the least deprived decile. Alcohol has been implicated as both a determinant and an outcome of socioeconomic inequality.
The ‘alcohol harm paradox’ refers to the phenomenon in which we observe greater alcohol-attributable morbidity and mortality among the most deprived socioeconomic groups compared to the least deprived groups, despite similar or lower average alcohol consumption among lower socioeconomic groups. Some explanations for the alcohol harm paradox include:
- different alcohol consumption patterns across socioeconomic groups;
- the multiplicative effect of alcohol use and other health behaviours;
- differential access to healthcare and treatment;
- inequalities in the social determinants of health; and
- substantial variation in the indicator used to measure socioeconomic status.
Alcohol use is associated with indicators across all five domains of the UK Public Health Outcomes Framework. Researchers have linked alcohol consumption with socioeconomic inequalities in life expectancy, violence, social and emotional wellbeing, child development, hospital admissions for various health conditions, alcohol-related cancers, infectious diseases and mortality.
While evidence-based and cost-effective policy interventions targeting alcohol availability, marketing, and affordability exist, there has been limited policy action on alcohol in recent years, particularly in England. Reducing the disproportionately high outlet density in deprived neighbourhoods and limiting the days and hours during which alcohol is sold have shown to reduce adverse health outcomes among lower socioeconomic groups. The recent implementation of minimum unit pricing in Scotland and Wales shows great promise in targeting heavy drinking and alcohol-related harms in lower socioeconomic groups. Increasing alcohol duty has the potential to benefit lower socioeconomic groups by decreasing the economic cost of alcohol-related harms and generating revenue that can be used to improve health and social services for disadvantaged groups.
Alcohol is not the only contributor to socioeconomic inequalities in the harms discussed. The multiplicative effects of poverty, stress, lack of access to health services, inadequate nutrition and lack of social capital, among many other risk factors, disproportionately affect those belonging to lower socioeconomic groups. The most effective and equitable method to eradicate health inequalities is to increase welfare spending designed to tackle the social determinants of health.
What are ‘health inequalities’?
In the UK, the term ‘health inequality’ is usually used to refer to systematic differences in health which are preventable and exist between socioeconomic classes or geographical areas, although there are other inequalities, for example by gender and ethnicity. Health inequalities can be defined in a purely descriptive way, but the moral and ethical dimensions of the term are often emphasised. The seminal 2010 Marmot Review, Fair Society, Healthy Lives, asserted: ‘The fact that in England today people in different social circumstances experience avoidable differences in health, well-being and length of life is, quite simply, unfair’ [1]. As an example, those living in the least deprived areas in Scotland live 22 to 24 years longer on average compared to those living in the most deprived area [2].
There is strong evidence to show that health inequalities are related to social determinants of health, such as housing, employment and poverty, rather than individual (biological or genetic) determinants [3,4]. Whitehead and Dahlgren defined social determinants of health as ‘the broad social and economic circumstances that together determine the quality of the health of the population’ [5]. These circumstances include intrapersonal (eg age, gender), interpersonal (eg social network), community- and organisational-level (eg education, health care services) and systems-level factors (eg policy environment).
Figure 1 Dahlgren and Whitehead’s model of the social determinants of health
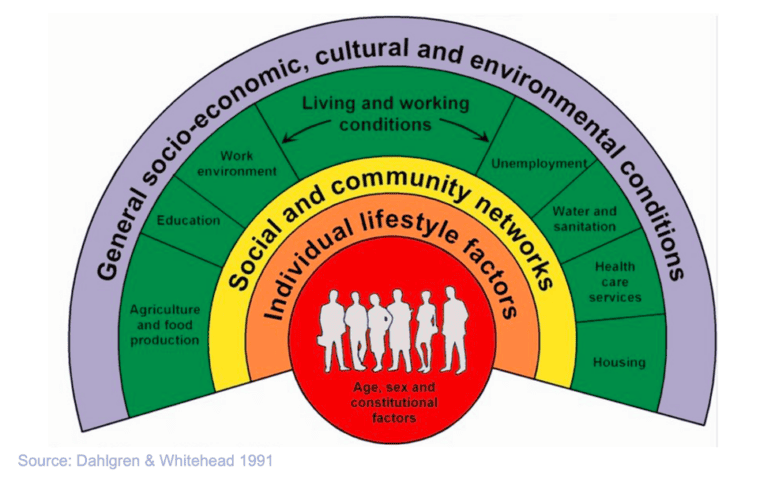
A number of pathways have been used to explain this link between social determinants of health and health inequalities. Those with lower socioeconomic status (SES) are more likely to be exposed to adverse environmental conditions, predisposing them to chronic health conditions. For instance, poorly maintained and damp housing has been shown to result in a greater likelihood of poor respiratory health in this population [6]. ‘Food deserts’, or areas deprived of adequate access to sufficient, affordable and nutritious food, are known to contribute to growing rates of obesity and cardiovascular disease among low-income communities in high-income countries [7]. Psychological factors such as stress responses and coping strategies have also been investigated as plausible pathways linking material inequalities to health inequalities [8].
Finally, cultural-behavioural factors such as alcohol consumption, smoking, exercise and diet are also implicated. Studies consistently find a socio-demographic gradient in the prevalence of multiple lifestyle-behavioural risk factors, with men, younger age groups and those of lower SES all more likely to experience multiple risks [9]. However, lifestyle-behaviours are generally regarded by researchers as both symptoms and causes of health inequalities. This is because such behaviours are themselves shaped by the socioeconomic contexts in which people live and work [10].
Progress made since the 2010 Marmot Review
The 2010 Marmot Review into health inequalities in England provided a snapshot of the impact that health inequalities have across a wide range of health and social issues. It found that:
- Infant mortality rates were 16% higher in children of routine and manual workers as compared to professional and managerial workers
- Deaths from cardiovascular diseases were 2.7 times higher in the 20% most deprived areas compared to the 20% least deprived
- Alcohol-related hospital admissions were 2.6 times higher amongst men and 2.4 times higher amongst women in the 20% most deprived areas compared to the 20% least deprived areas
In February 2020, the Institute of Health Equity published a report exploring changes in health inequalities and national policy action since the release of the 2010 Marmot Review [11]. This report found that, rather than seeing improvements, socioeconomic inequalities in health have either persisted or worsened in the UK. For instance, increases in life expectancy have slowed down with the greatest slowdown observed in the most deprived areas, especially in the north of England. Furthermore, health and social inequalities between men and women are worsening. Those living in the most deprived areas, especially women, spend more time in ill health. A decade of austerity measures following the 2008 financial crisis has defunded initiatives meant to reduce health inequalities, such as Sure Start Children’s Centres, in the most disadvantaged areas. In fact, deprived areas have experienced the most disinvestment per person compared to more affluent areas.
The relationship between alcohol and health inequalities
There is a substantial evidence base identifying links between alcohol and health inequalities. In 2017, those in the most socioeconomically deprived decile had 2.23 times the rate of alcohol-specific mortality (ie deaths wholly due to alcohol use) and 1.53 times the rate of alcohol-related mortality (ie deaths partially due to alcohol use) compared to the least deprived decile [12]. One study covering the West of Scotland concluded that ‘exposure to disadvantaged social circumstances across the life course, but particularly in adulthood, is associated with detrimental patterns of alcohol consumption and problem drinking in late middle age,’ presumably leading to a greater alcohol-attributable burden among lower socioeconomic groups [13]. However, there are many issues in need of greater clarification. Alcohol-related health inequalities are more complicated than for other drugs, such as tobacco, and somewhat paradoxical. Lower socioeconomic status (SES) is associated with higher morbidity and mortality for alcohol-attributable causes – despite lower socioeconomic groups usually reporting lower average levels of alcohol consumption [14].
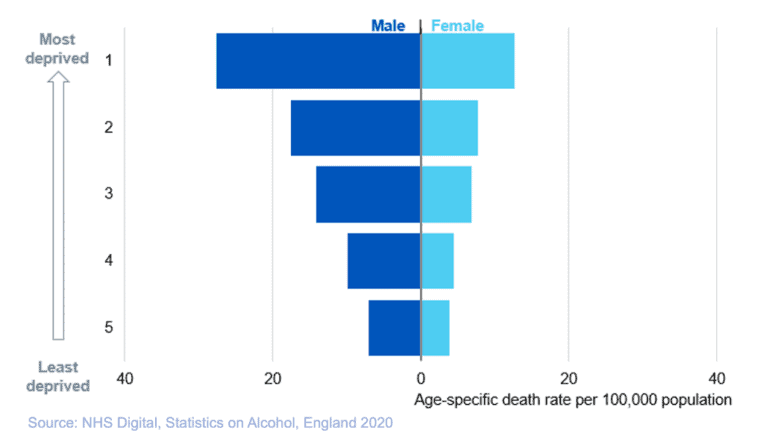
As figures 2 and 3 below show, the proportion of higher risk drinkers declines as levels of deprivation increase, yet alcohol-specific mortality moves in the opposite direction and grows with deprivation. This phenomenon is referred to as the ‘alcohol harm paradox’: why should some groups experience worse alcohol-related harms, despite apparently consuming less alcohol?
Figure 2 Proportion of adults drinking at increased or higher risk of harm, by Index of Multiple Deprivation and sex
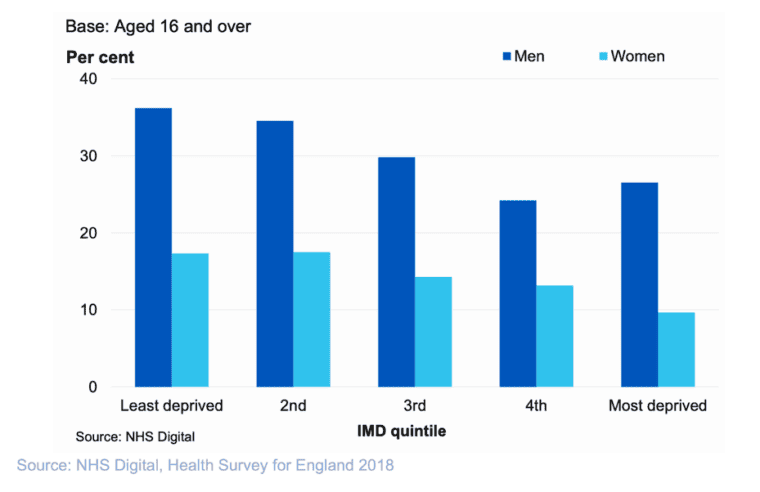
Figure 3 Alcohol-specific mortality per 100,000 persons by deprivation quintile
The alcohol harm paradox
The alcohol harm paradox refers to the phenomenon in which we observe greater alcohol-attributable morbidity and mortality among the most deprived socioeconomic groups compared to the least deprived groups, despite similar levels of alcohol consumption or a lower average consumption among lower socioeconomic groups. A number of explanations exist for the alcohol harm paradox; however, no single proposed causal mechanism is able to fully explain this phenomenon and the body of evidence for these mechanisms is at times conflicting.
Consumption patterns differ along the social gradient
One explanation could be that people living in more difficult circumstances—despite drinking less on average as a whole—consume alcohol in more harmful ways (ie more frequent and higher intensity of drinking sessions), suggesting that interactions with other lifestyle-behaviours and health determinants and/or cultural differences may be important. Lewer et al showed that those of higher SES were more likely to exceed the recommended number of drinks per week (14 drinks for women and 21 drinks for men) [15]. However, those of lower SES, as measured by income, education level, occupation, and neighbourhood deprivation, were more likely to report exceeding the highest drinking thresholds (60-85+ drinks per week among women and 80-110+ drinks per week among men). This gradient reversal indicates that lower SES groups have a greater proportion of light drinkers and abstainers and also very heavy drinkers. With regards to heavy episodic drinking, those with lower-level education qualifications, lower status occupations and living in the most deprived areas were more likely to exceed the highest drinking thresholds in one drinking session.
Yet, the evidence supporting consumption patterns as a full explanation for the alcohol harm paradox is mixed. Katikireddi et al found that, even after adjusting for consumption and binge drinking, alcohol-attributable harms in lower SES groups occur at almost three times the rate of harms in higher SES groups [16]. So, if consumption patterns do play a role in alcohol-related health inequalities, they do not fully explain the alcohol harm paradox and other factors must also be considered.
Alcohol use overlaps with other health behaviours
Some research has looked at alcohol consumption as part of a complex system of interactions with other ‘poly-behaviours’, such as diet and exercise, which account for the relatively greater harms that are experienced by more deprived groups. Research by the Kings Fund into how patterns of multiple lifestyle risks (ie smoking, excessive alcohol use, poor diet and low levels of physical activity) spread across socioeconomic groups, found that people with no qualifications were five times more likely to engage in all four unhealthy behaviours than those with higher education [17]. It was found that engaging in all four unhealthy behaviours resulted in a 14-year reduction in life expectancy compared with those who engaged with none of them [18].
Other research has gone further and investigated how some of these unhealthy behaviours might interact with each other. Researchers looking at obesity and alcohol consumption have found a ‘supra-additive interaction’ between the two, particularly in relation to liver disease.16 It is also known that a combination of smoking and drinking accelerates the risk of mouth and throat cancers, and that premature mortality is particularly high in smokers who drink more than 15 units a week [19]. It has been found that alcohol-related head and neck cancers in the UK are 2-3 times more common in the most disadvantaged groups compared to the least disadvantaged [20,21].
However, Katikireddi et al have shown that adjusting for smoking and BMI at the individual level only slightly explains the relationship between SES and alcohol-related harms in a large, cross-sectional sample of Scottish residents [22]. Interestingly, an Australian study looking at the relationship between alcohol-related harms and risk-taking behaviours (eg drink driving, property damage, verbal and physical altercations) across SES groups found that those of higher SES engaged in these behaviours at a higher rate compared to those of lower SES [23]. According to this study, engaging in risky behaviour while drinking does not seem to contribute to greater harms in lower SES groups. Therefore, although there is some evidence for a multiplicative effect of unhealthy behaviours on alcohol-related harms, we must also consider other underlying mechanisms of the alcohol harm paradox.
There is a social gradient in access to health care and help-seeking behaviours
There is also evidence that those living in more deprived circumstances face greater barriers to accessing health and alcohol-related services and interventions than those in less deprived circumstances [24]. Barriers include factors such as costs, distance, transport and availability, and stigmatisation, with stigma a particular problem for those of low SES [25]. In addition, those from a more deprived background with insecure employment may be less able to take time off work when they get ill, compounding the problem [26]. Alternatively, those receiving additional help or benefits related to a long-term health condition or disability may be discouraged from efforts to get better by the fact that they would then have to go without this additional help. In either scenario individuals may become trapped in a situation that puts them at risk of poor health [27].
Wider social determinants of health have a role in alcohol-related harms
As noted earlier, one of the most well-supported explanations for overall health inequalities relates to the material (social, economic and environmental) circumstances in which people live and work—the social determinants of health [28,29]. These factors also seem likely to contribute to explaining alcohol-related inequalities and, potentially, the alcohol-harm paradox. For example, in reflecting on why lower educated groups are more likely to report negative consequences of alcohol than higher educated groups, even after controlling for drinking patterns, some researchers suggest that ‘those of fewer resources are less protected from the experience of a problem or the impact of a stressful life event’ [30].
Qualitative case studies of heavy drinkers aged 18–24 years of age in a socioeconomically disadvantaged area of Melbourne, Australia point to interrelated ‘social forces’, including ethnic and family patterns and drinking settings, as factors that must be considered. The report states that it is incorrect to think that ‘alcohol acts in stable and predictable ways, while ‘social factors’ play a role in attenuating or amplifying this intensity,’ and researchers should instead think about how intersecting social forces ‘transform alcohol effects so that the quantity of alcohol consumed ceases to be a good predictor of the outcome.’
Measuring socioeconomic status and its relationship with alcohol-related harms is complex
Simply using one or a few indicators of SES in isolation may be insufficient in explaining its impact on alcohol-related morbidity and mortality. Commonly used measures of SES, such as household income, employment status and education, often intersect with each other in unique ways and also intersect with race and ethnicity, gender and other social constructs [31]. Therefore, we can expect these different intersections to be associated differently with alcohol-related harms.
Some studies have attempted to overcome this issue using composite scores for SES based on multiple indicators, but interpretation of these scores can be difficult [32,33]. One study of South East London identified six distinct socioeconomic groups using the intersection of income, occupation, housing status and education indicators and explored the relationship between these groups and hazardous, harmful, and dependent drinking [34]. The authors found that economically inactive renters, economically inactive homeowners, and professional renters were more likely to drink at harmful/dependent levels compared with professional homeowners, pointing to different underlying mechanisms of alcohol use according to intersecting socioeconomic factors. This study demonstrates value in using an intersectional approach to define categorical rather than ordinal socioeconomic groupings to examine differences in alcohol use and outcomes, which also has great implications for equity in alcohol research.
Why should we address alcohol-related health inequalities?
The impact of alcohol-related inequalities in health has clear public policy implications. A 2016 report published by Public Health England showed that alcohol-related harms costs the UK approximately £27–£52 billion per year, and related morbidity and mortality in lower SES groups are disproportionately contributing to costs [35]. More generally, health inequalities cost the UK £31–33 billion per year in terms of illness, lost taxes and productivity, in addition to £20–32 billion per year in social security payments that are due to poor health [36].
These costs are not purely economic; people living in deprived areas experience first-hand the burden of alcohol harms more than any other group. Alcohol is involved in a wide range of health and social concerns, from dangerous driving to crime and domestic abuse, cancer, heart and liver disease, to accidents at work. Given this, and the fact that the most deprived communities are disproportionately affected by these issues, tackling problems associated with alcohol can be seen as central to efforts to reduce health inequalities across society, whilst tackling the ‘upstream’ social, economic and environmental determinants of health inequalities is likely to support efforts to reduce alcohol-related harms [37,38].
Most importantly, to quote Michael Marmot [39]:
We do have an ideological position: health inequalities that could be avoided by reasonable means are unfair. Putting them right is a matter of social justice.
UK Public Health Outcomes Framework
The UK Public Health Outcomes Framework (PHOF) is a collection of health indicators across five domains (overarching indicators, wider determinants of health, health improvement, health protection and health care and premature mortality) that provides the government, health professionals, and the public with a framework through which to assess improvements or declines in various health outcomes and, consequently, socioeconomic inequalities in these outcomes [40].
Alcohol-related factors are found across all five of the domains in the current PHOF for England and, as such, tackling alcohol-related harm could be a key route to reducing health inequalities in general. This briefing will use the 2020 PHOF as a guide for exploring alcohol-related health inequalities across socioeconomic groups and will inform potential policy actions related to minimising socioeconomic inequalities in alcohol-related harms.
Alcohol-related health inequalities across socioeconomic groups
Overall health and life expectancy
Life expectancy
In the UK, life expectancy at birth and healthy life expectancy at birth, or the number of years one can expect to live without illness, show a social gradient [41]. Those living in the most deprived neighbourhoods are expected to live for 7.7 (female) – 9.5 (male) fewer years on average compared to those in more affluent neighbourhoods. Moreover, in addition to shortened life expectancy, those living in the most deprived areas spend 30-34% of their lives on average with a long-term illness compared to 15-18% of those living in the least deprived areas. Since 2010, improvements in life expectancy have mostly stagnated, and inequalities in life expectancy and healthy life expectancy between lower and higher socioeconomic groups have widened, especially among women.
Rehm and Probst have consistently linked alcohol consumption, at least in part, to the observed differentials in life expectancies [42,43,44]. Alcohol use is a major risk factor for non-communicable diseases (eg cardiovascular disease, cancer, etc.), infectious diseases, and unintentional and intentional injuries [45]. One study of premature deaths in England found that among the largest contributors to socioeconomic inequalities in life expectancy were tuberculosis, opioid use, HIV, psychoactive drug use and viral hepatitis, which are all strongly associated with alcohol use [46].
Social determinants of health
Interpersonal violence
Interpersonal violence has strong evidence for a social gradient, especially among adolescent and young adult men [47,48]. Interpersonal violence is defined as an act of physical aggression between family members, friends, acquaintances, and strangers. A five-year ecological study in England showed that those living in the most deprived areas had five and a half times higher odds of being admitted to the hospital after a violent incident compared to those living in the least deprived area [49].
There is strong evidence showing a link between alcohol consumption and violence. One of the World Health Organization’s (WHO) recommended strategies to prevent and reduce violence is ‘reducing the availability and harmful use of alcohol’ [50]. In fact, the WHO describes harmful alcohol use as both a determinant and outcome of violence.
A 2020 report published by the Institute of Alcohol Studies (IAS) found that lower socioeconomic groups experience up to five and a half times the prevalence of alcohol-related violence compared to higher socioeconomic groups and up to 14 times the incidence. Also, patterns of alcohol-related violence across socioeconomic groups in the UK and Wales are different after disaggregating domestic, stranger, and acquaintance violence [51]. Those with the lowest annual household income (< £19,999), unemployed, and social renters were significantly more likely to have experienced domestic and acquaintance violence compared to those of higher SES. In contrast, these groups were least likely to experience alcohol-related victimisation by a stranger [52].
Intimate partner violence
Intimate partner violence (IPV) includes ‘physical, sexual, and emotional abuse and controlling behaviours by an intimate partner’ [53]. A study of all European Union member states examining the relationship between SES and intimate partner victimisation of women only in heterosexual couples found that the lower educational qualifications of the perpetrator and victim and the perpetrator’s lower income level were significantly associated with IPV [54]. Importantly, men who misused alcohol more than once per week were more likely to perpetrate IPV.
The IAS report discussed in the previous section established that the high prevalence and incidence of domestic violence in lower socioeconomic groups, much of which can be classified as intimate partner violence, may explain socioeconomic patterns in overall alcohol-related violence [55].
Antisocial behaviour other than violence
The IAS report examining inequalities in victimisation also assessed alcohol-related antisocial behaviour (ASB), such as drunken noise, street harassment, and other harms related to others’ drinking [56]. It found that people from the lowest SES groups (annual income < £19,999, social renters, and never working/long-term unemployed) were more likely to experience ASB frequently. Previous work at IAS has also shown that 16.1% of people in skilled, working, and nonworking social classes compared to 7.0% in the middle class are more likely to report problems with friends and neighbours as a result of others’ drinking [57]. Also, a study of alcohol-related complaints in New York City discovered that more deprived neighbourhoods had an increased likelihood of alcohol-related complaints (eg noise, illegal use, etc) [58].
Homelessness
People experiencing homelessness have historically been excluded from studies of socioeconomic inequalities [59]; however, it is argued that these individuals comprise their own socioeconomic group with distinct health behaviours, alcohol-related outcomes, and health needs that must be researched to ultimately close the gap in health inequalities. A 2015 study of homelessness and alcohol use in the UK found that those who are experiencing homelessness drank 97.1% (males) – 222.1% (females) more units per week compared to the general population [60]. A qualitative study of 26 people experiencing homelessness in North West England demonstrated how, for some, a bidirectional relationship between heavy alcohol use and other adverse life experiences led to social isolation and a breakdown of relationships, ultimately leading to homelessness [61]. One participant described his lived experience as follows:
I used to drink to get rid of the anxiety and also to numb the pain of the breakup of me marriage really, you know it wasn’t good, you know. One thing led to another and I just couldn’t stop me alcohol… it was like I either stop drinking or I had to move out of me mum’s. I lost me job in the January through being over the limit in work from the night before uum so one thing led to another and I just had to leave.
Health outcomes over the life course
Child health and development
The alcohol harm paradox is not restricted to harms experienced by young and older adults. Studies have found that, while pregnant, women of lower SES consume alcohol less frequently on average compared to women of higher SES, yet rates of low birth weight, foetal alcohol spectrum disorder (FASD), and other child developmental health problems associated with prenatal and perinatal alcohol use are higher among those of lower SES [62].
This paradox may be explained by a higher prevalence of heavy drinkers [63] and the multiplicative effect of smoking, poverty, inadequate nutrition, stress and lack of access to prenatal care among mothers belonging to lower SES groups [64,65,66].
Parental SES in childhood strongly predicts alcohol-related morbidity and mortality in young adulthood [67]. A Swedish retrospective cohort study of 948,518 individuals found that children born to parents in unskilled manual positions had 2.24 times the risk of experiencing an alcohol-related health problem in young adulthood and that parental substance use attenuated this effect only slightly. It is possible that limited socioeconomic capital throughout childhood, adolescence and adulthood among this population contributes to the observed alcohol-related inequalities.
Alcohol-related hospital admissions
Rates of alcohol-related hospital admissions – that is, the number of hospital admissions attributed to the acute or chronic impacts of alcohol use – shows a clear social gradient by area deprivation (see figure 4). According to Public Health England, the number of alcohol-related admissions in the most deprived decile in fiscal year 2017/2018 was 2,839 per 100,000 persons compared to 1,814 per 100,000 persons in the least deprived decile.
Figure 4 Admission episodes for alcohol-related conditions by deprivation decile in 2017/18 (per 100,000 persons)
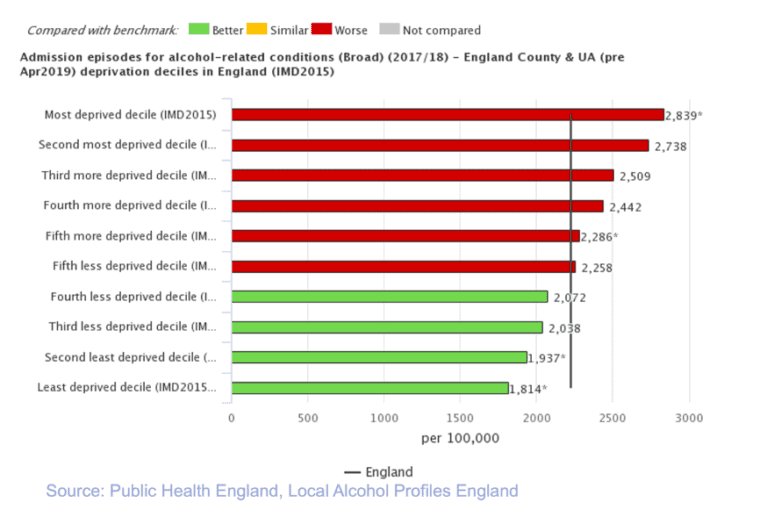
Sadler et al demonstrated how this socioeconomic gradient is seen for acute and chronic conditions wholly attributable to alcohol (eg poisoning, alcohol liver disease) and acute conditions partially attributable to alcohol (eg assault, self-harm, unintended injuries) [68]. Furthermore, the gradient was steeper for acute conditions wholly attributable to alcohol, with lower SES groups more likely to experience these harms.
Green et al examined changes in these phenomena over time and found a relative increase of alcohol-related hospital admissions compared to an increase in unrelated admissions from 2002/03 to 2013/14 [69]. Their findings reflect Sadler et al, in that acute admissions wholly attributable to alcohol had the largest relative increase in the most deprived quintile. Over time, there have been widening inequalities in acute hospital admissions wholly attributable to alcohol use, mental and behavioural disorders related to alcohol use, and intentional self-poisoning, with those in the most deprived groups disproportionately affected.
Alcohol-related cancers
According to Public Health England, the incidence – the number of new diagnoses – of alcohol-related cancers (ie cancers of the mouth and throat, oesophagus, colon and rectum, liver, and breast) from 2015-2017 was higher in the most deprived decile (41.36 per 100,000 persons) compared to any other decile (see figure 5).
Figure 5 Average incidence of alcohol-related cancers by deprivation decile from 2015-17 (per 100,000 persons)
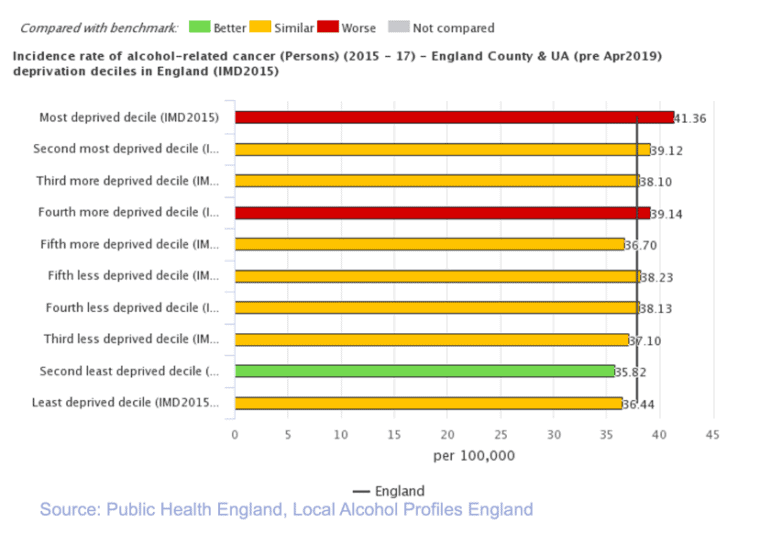
Behind the overall incidence rates of alcohol-related cancers, there are different social gradients in different cancers. For example, breast cancer is more common among higher SES groups [70]. Alcohol consumption, independent of other risk factors, is significantly associated with head and neck cancers [71,72]. A systematic review of the effect of SES on the risk of head, neck and oesophageal cancers found that low income, low occupational class, and low educational attainment were associated with an increased risk of oral cancer, with those in the lowest income group having 2.41 times the risk of having oral cancer [73]. The authors posited that lifestyle factors, including heavy alcohol use, likely contribute to the observed inequality, as they themselves are present on a social gradient.
A study comparing Western European populations suggested that alcohol use substantially influences socioeconomic inequalities in male cancer mortality in France, Spain and Switzerland but not in the Nordic countries and nor in Belgium [74]. In fact, inequalities in alcohol-related cancers accounted for 29-36% of the overall socioeconomic inequalities in cancer mortality in France and Spain and only 5-15% in Belgium and the Nordic countries. The authors hypothesised that this may be due to higher levels of daily consumption in the Southern European countries compared to the Nordic countries.
Alcohol-related injuries
As previously discussed, intentional injuries as a result of concurrent alcohol use and violence show a strong social gradient, with lower SES groups at increased risk [75]. A similar but less pronounced gradient exists for alcohol-related unintentional injuries, such as falls and road traffic accidents [76]. The most deprived decile experiences higher rates of hospital admissions for alcohol-related unintentional injuries (164.7 admissions per 100,000 persons) compared to the least deprived deciles (133.6–139.3 admissions per 100,00 persons) (see figure 6).
Figure 6 Admission episodes for alcohol-related unintentional injuries in 2017 (per 100,000 persons)
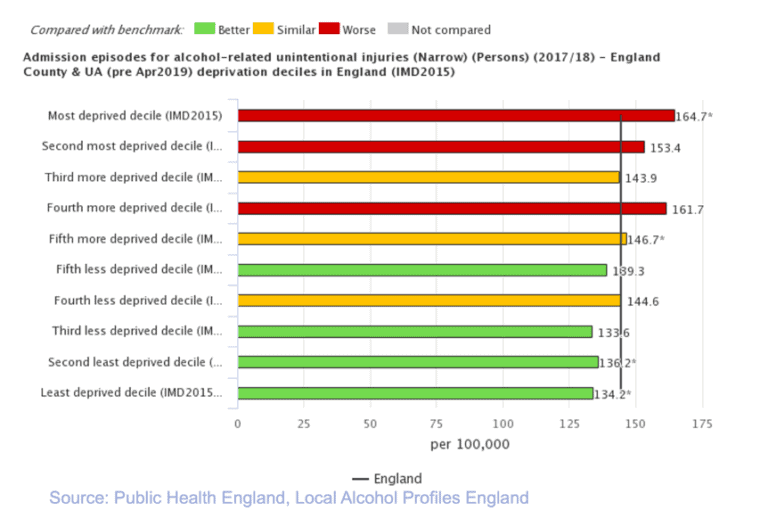
One specific and common example of intentional injuries are facial injuries sustained as a result of alcohol-related interpersonal violence, mostly affecting young men belonging to lower SES groups [77,78]. A Scottish study of 22,417 hospital encounters of alcohol-related facial injuries showed that patients from the most deprived areas were almost 7 times as likely to sustain a facial injury compared to those living in more affluent areas [79].
Alcohol-related injuries can have both acute and long-term chronic effects. A nationwide study of almost 1 million adolescents using linked NHS Hospital Episode Statistics with mortality data found that adolescent boys admitted for a drug- or alcohol-related injury had 4.51 times the risk of suicide and 4.91 times the risk of drug- or alcohol-related deaths in later life compared to boys admitted for accidental injury [80].
Alcohol-related outcomes after incarceration
As of 2016, around three quarters of incarcerated or otherwise justice-involved individuals in the UK have a problem with alcohol, and over a third are dependent on alcohol [81]. It has been established that this population has often experienced socioeconomic disadvantage [82]. The immediate period after incarceration is critical in minimising the harms associated with heavy alcohol use, as studies have shown that mortality from drug- or alcohol-related causes is especially high in the years following release [83]. A longitudinal study in Sweden of 47,326 individuals post-incarceration showed that, after controlling for possible confounders, those with alcohol use disorder had an increased rate of all-cause mortality [84]. Treatment and other interventions addressing alcohol use disorder in the critical period after incarceration may not be reaching this marginalised population, exacerbated by the limited socioeconomic capital available to this group as a result of factors prior to and after incarceration.
Self-reported well-being
A study using a stratified random sample of 15,228 individuals residing in the North West of England established that heavy drinkers in the most deprived tertile in the North West of England were at the highest risk of reporting low life satisfaction [85]. Additionally, a nationally representative study of Finnish adolescents found that, although alcohol use among adolescents has decreased since the early 2000s, those who had parents who were unemployed and with lower levels of education remained more likely to consume alcohol frequently and binge drink and were more likely to report depressive symptoms [86]. This study showed that the inequalities in self-reported mental well-being between adolescents belonging to lower socioeconomic groups and those in higher socioeconomic groups had increased over time.
Preventing infectious disease
Sexually transmitted infections
Increased alcohol use is causally related to an increased rate of sexually transmitted infections, particularly human immunodeficiency virus (HIV) infections, across the world [87,88,89]. Alcohol can lead to risky sexual behaviours and has been linked to poor health outcomes and nonadherence to anti-retroviral medications among those with HIV/AIDS [90,91]. A systematic review and meta-analysis of African countries found that heavy drinkers were 2.04 times more likely to be HIV-positive than non-drinkers [92], and another study in South Africa found that the interaction between alcohol consumption and low SES was associated with a higher likelihood of HIV infection than what would be expected from the product of both factors individually. This effect could be attributed to other risk factors, such as malnutrition and co-infections, that are present at the intersection of alcohol use and low SES.
Tuberculosis
There is good evidence of a causal relationship between heavy alcohol use and TB; a systematic review and meta-analysis exploring this relationship found that heavy drinkers have 2.94 times the risk of contracting TB compared to light drinkers and abstainers. Alcohol can have immunosuppressive effects, leaving heavy drinkers unable to ward off TB infection and also allowing for rapid disease progression among those who already have TB. Furthermore, the social determinants of poor health impacting those with lower SES and living in more deprived areas, namely poverty, unsafe living conditions and malnutrition, allow for increased TB transmission and increased susceptibility to infection [93,94].
Preventable and premature mortality
Alcohol-related mortality
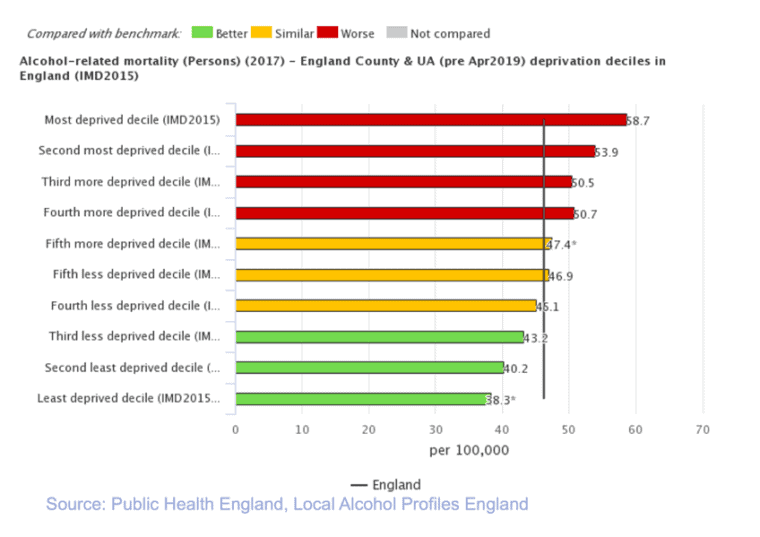
In England, rates of both alcohol-specific mortality (ie deaths solely due to alcohol use) and alcohol-related mortality (ie deaths attributable to alcohol use in part) show a clear social gradient by deprivation decile (figures 7 and 8) [95]. On average per year, 16.5 per 100,000 persons in the most deprived decile compared to 7.4 per 100,000 persons in the least deprived decile died as a result of alcohol-specific causes from 2014–2016. Similarly, 58.7 per 100,000 persons in the most deprived decile compared to 38.3 per 100,000 persons in the least deprived decile died as a result of alcohol-related causes in 2017.
Figure 7 Average alcohol-specific mortality from 2015-17
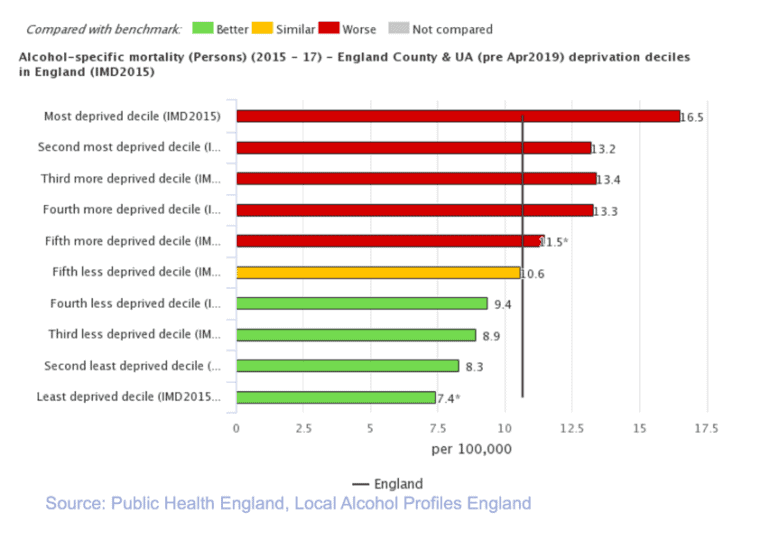
Figure 8 Alcohol-related mortality in 2017
Studies have shown that lower SES is associated with an increased risk of alcohol-attributable cardiovascular disease, including coronary heart disease and stroke.18 In fact, one study of 17 European countries found that smoking and alcohol are the largest contributors to the observed socioeconomic inequalities in all-cause mortality, with the largest contribution found in cardiovascular disease and external cause mortality [96]. As previously discussed, alcohol also accounts for a large portion of inequalities in cancer and liver disease mortality [97]. The most comprehensive review of alcohol-related mortality and SES published thus far found that 27% of the socioeconomic inequalities in mortality can be explained by variation in alcohol consumption [98]. Overall, individuals belonging to lower socioeconomic groups face anywhere between 3.8–5.2 times the risk of alcohol-attributable mortality compared to those in higher socioeconomic groups.
Suicide
The rate of suicide in the most deprived decile (13.3 per 100,000 persons) is much higher than in any other decile [99]. A number of risk factors in those residing in the most deprived areas have been implicated, including social isolation, lack of opportunity and social mobility, poverty, mental health disorders and substance use disorders.
Some experts have hypothesised that alcohol use may act as a mediator between social stress and suicide, whether it is in the form of chronic alcohol use disorder or acute and heavy alcohol consumption immediately prior to suicide [100]. A study of European Union member states found a significant relationship between the unemployment rate and alcohol-involved suicides among adolescent women [101]. Also, a nationally representative study of women in Finland found that low income, social class, and educational qualifications were strongly associated with alcohol-associated suicides [102]. Moreover, the link between violence and alcohol use in lower socioeconomic groups is thought to contribute to increased suicides among adolescent and young men of lower SES [103].
Policy interventions to address alcohol-related inequalities
Alcohol has a wide and significant impact across a range of issues related to health inequalities, and therefore is central to attempts to narrow health inequalities overall. However, health bodies have argued that policy efforts to achieve this in the UK are lacking.
Whilst the Coalition Government has given the NHS a legal duty to reduce inequalities in access to care, critics have argued it now has less responsibility for tackling overall inequalities in health [104]. The Public Health Outcomes Framework includes a commitment to ‘reduce differences in life expectancy and healthy life expectancy between communities’ [105], but, as the 2020 Marmot review has demonstrated, initiatives designed to reduce health inequalities have been defunded and the national government has not committed to a comprehensive plan to reduce health inequalities going forward [106].
The spread of alcohol-related indicators across all four domains suggests that clear and effective efforts to reduce alcohol-related health inequalities have the potential to make a significant impact on health inequalities across the board. However, critics have argued that while evidence-based policy initiatives targeting alcohol availability, marketing, and affordability exist, there has been limited policy action on alcohol in recent years, particularly in England. In addition to alcohol-specific measures, it is important to note that general welfare spending has been found to impact positively on alcohol-attributable mortality. Several studies have shown that a rise in social welfare spending is associated with a decrease in alcohol-attributable mortality, whereas rising health care spending is not [107].
Alcohol availability and outlet density
Alcohol availability and outlet density have been found to be associated with increased consumption, heavy drinking, and drink-related problems as well as increased violence [108,109,110]. This is thought to be because of the relationship between density and price, with geographically close outlets competing with each other to attract customers and increasing the ease and convenience with which people can access alcohol [111]. In addition, clustering of premises can lead to a greater potential for violence in the night time environment, and a diversification of bar types can result in heavier drinkers tending to end up in the same place, again increasing the risks of violence and of normalising heavier drinking [112].
Research in Scotland has also found a relationship between off-licence density and crime, with deprived areas more likely to be affected [113]. Other research identified that neighbourhoods with greater concentrations of alcohol outlets had significantly higher alcohol-related hospitalisations and deaths and that mortality in deprived neighbourhoods with higher off-sales outlet densities was much higher [114]. Importantly, the individual-risk factors associated with lower SES, such as poverty and lack of economic opportunity, may compound vulnerability to increased alcohol outlet density [115,116].
Addressing the density of premises is not an easy task. In England and Wales, cumulative impact policies (CIPs) can be introduced in areas where the cumulative effect of licensed premises on the four licensing objectives is sufficient to suggest that the growth of similar premises in that area needs to be controlled. While it introduces an assumption that no further licences will be granted unless the applicant can show that it will not add to the existing problems, it does not necessarily allow for the current density to be reduced, even if it is already a problem [117].
Another strategy to limit alcohol availability is to reduce the days and hours of sale [118]. A systematic review found that reducing the hours of sale was associated with decreased alcohol consumption, alcohol-related road traffic accidents and alcohol-related injuries and assaults in some settings [119].
Alcohol marketing and advertising
Alcohol industry marketing and advertising tactics are known to increase the appeal of drinking by modifying social and cultural norms surrounding drinking and glamorising it, especially among young people [120,121]. It is possible that alcohol marketing disproportionately targets those belonging to lower socioeconomic groups, as this population is more likely to be exposed to advertisements outside of alcohol outlets in deprived neighbourhoods and on television [122,123].
Alcohol affordability and minimum unit pricing
There is strong evidence that reducing the affordability of alcohol by raising prices leads to a reduction in alcohol consumption and associated mortality and morbidity, as well as a reduction in levels of violence and crime [124,125]. One such price-related policy is minimum unit pricing, which sets a level below which retailers are not allowed to sell alcohol, depending on the number of units it contains. The evidence base for minimum unit pricing has been supported by the World Health Organisation and the Organisation for Economic Co-operation and Development and has been described as the most cost-effective strategy to minimize alcohol-related harm.
In 2018, Scotland implemented a minimum unit price of 50p per UK unit and in 2020 Wales implemented one at the same level. Although research examining the health-related impacts of the policy in Scotland is still emerging, a recent study evaluating its most proximate impacts found that weekly purchases of alcohol reduced by 9.5 g per household on average and that this reduction was greatest in low income households [126]. The study also found that the increase in purchase price was highest in low income households, but any increases in weekly expenditures were associated with increasing household purchases and were not systematically associated with income level. In sum, minimum unit pricing in Scotland has proven to target alcohol purchases in the top fifth of alcohol purchasing households only. Further research must assess the impact on the most deprived households with very heavy drinkers to ascertain whether it has increased the economic burden on these households and whether this policy is causally linked with diminishing alcohol-related harms in lower socioeconomic groups.
Another approach to reducing the affordability of alcohol is increasing alcohol duty. An IAS report published in 2020 estimated the economic burden of alcohol duty on different socioeconomic groups using both household income and expenditures [127]. It found that duties on beer, spirits and cider may be slightly regressive (ie lower socioeconomic groups pay a slightly higher share of their expenditures on alcohol), especially among young men. However, lower income households may also be more sensitive to price changes and may consequently change their purchasing habits. Furthermore, extra revenue generated from increased alcohol duty could be used to directly benefit lower socioeconomic groups through government spending on health programs or tax cuts for those in low-income households, for example, which would make an alcohol duty progressive. Increased alcohol duty can also address the alcohol harm paradox by decreasing overall consumption and, as a result, minimising the disproportionate burden of alcohol-related harms among lower socioeconomic groups.
General welfare expenditure
In addition to alcohol control policies, it is important to note that general welfare spending has been found to impact positively on alcohol-attributable mortality. Several studies have shown that a rise in social welfare spending is associated with a decrease in alcohol-attributable mortality, whereas rising health care spending is not [128]. As stated by the King’s Fund [129]:
The impacts of the government’s social welfare reforms, the recession and long-term unemployment have the potential to outweigh any efforts the NHS and local authorities may make to reduce inequalities. If the government is serious about narrowing health inequalities, it cannot rely on the NHS and public health sector alone.
Since 2010, not only has overall funding in health and social programs in the UK decreased, funding allocated towards socioeconomically deprived areas has decreased disproportionately and has further exacerbated inequity and health inequalities [130]. The idea of ‘proportionate universalism’ describes how ‘greater intensity of action is likely to be needed for those with greater social and economic disadvantage, but focusing solely on the most disadvantaged will not reduce the health gradient, and will only tackle a small part of the problem’ [131].
- Marmot M (2010), Fair Society, Healthy Lives: The Marmot Review. The Marmot Review; 2010
- Public Health Scotland, What are health inequalities?
- Marmot M, Wilkinson R (2005), eds. Social Determinants of Health. 2nd ed. OUP Oxford
- WHO Commission on Social Determinants of Health, Organization WH (2008), Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health : Commission on Social Determinants of Health Final Report. illustrated. World Health Organization.
- Whitehead M, Dahlgren G (1991), What can be done about inequalities in health? Lancet. 338(8774): 1059-1063. doi:10.1016/0140-6736(91)91911-d
- Thomson H, Thomas S, Sellstrom E, Petticrew M. The health impacts of housing improvement: a systematic review of intervention studies from 1887 to 2007. Am J Public Health. 2009; 99 Suppl 3: S681-92. doi:10.2105/AJPH.2008.143909
- Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966-2007. Prev Chronic Dis. 2009; 6(3): A105
- Probst C, Roerecke M, Behrendt S, Rehm J (2014), Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol. 43(4): 1314-1327. doi:10.1093/ije/dyu043
- Buck D, Frosini F (2012), Clustering of Unhealthy Behaviours over Time: Implications for Policy and Practice. The King’s Fund
- Shaw M (2004), Health Inequality: An Introduction to Theories, Concepts and Methods. Mel Bartley. Cambridge: Polity Press, pp. 224, 16.99 (PB), ISBN: 0745627803. Int J Epidemiol. 2005; 34(2): 500-502. doi:10.1093/ije/dyi053
- Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J (2020) Health Equity in England: The Marmot Review 10 Years On. Institute of Health Equity
- Local Alcohol Profiles for England (2020) Public Health Profiles
- Anderson P, Baumberg B (2006), Alcohol in Europe: A Public Health Perspective. Institute of Alcohol Studies
- Anderson P, Baumberg B. Alcohol in Europe: A Public Health Perspective
- Lewer D, Meier P, Beard E, Boniface S, Kaner E (2016), Unravelling the alcohol harm paradox: a population-based study of social gradients across very heavy drinking thresholds. BMC Public Health; 16: 599. doi:10.1186/s12889-016-3265-9
- Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH (2017), Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health; 2(6): e267-e276. doi:10.1016/S2468-2667(17)30078-6
- Anderson P, Baumberg B. Alcohol in Europe: A Public Health Perspective
- Probst C, Roerecke M, Behrendt S, Rehm J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis
- Marmot M (2010), Fair Society, Healthy Lives: The Marmot Review
- Conway DI, Petticrew M, Marlborough H, Berthiller J, Hashibe M, Macpherson LMD (2008), Socioeconomic inequalities and oral cancer risk: a systematic review and meta-analysis of case-control studies. Int J Cancer; 122(12): 2811-2819. doi:10.1002/ijc.23430
- Jones L, Bates G, McCoy E, Bellis MA (2015), Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health; 15(1): 400. doi:10.1186/s12889-015-1720-7
- Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH (2017), Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data
- Livingston M (2014), Socioeconomic differences in alcohol-related risk-taking behaviours. Drug Alcohol Rev; 33(6): 588-595. doi:10.1111/dar.12202
- Moscelli G, Siciliani L, Gutacker N, Cookson R (2018), Socioeconomic inequality of access to healthcare: Does choice explain the gradient? J Health Econ. 57: 290-314. doi:10.1016/j.jhealeco.2017.06.005
- Impinen A, Mäkelä P, Karjalainen K, et al (2011), The association between social determinants and drunken driving: a 15-year register-based study of 81,125 suspects. Alcohol Alcohol. 46(6): 721-728. doi:10.1093/alcalc/agr075
- Violence & Socioeconomic Status (2010), American Psychological Association
- Anderson P, Baumberg B, (2006).
- Whitehead M, Dahlgren G (1991), What can be done about inequalities in health? Lancet.
- Lorenc T, Petticrew M, Welch V, Tugwell P (2013), What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 67(2): 190-193. doi:10.1136/jech-2012-201257
- Probst C, Roerecke M, Behrendt S, Rehm J (2014)
- See references 25–27
- Beard E, Brown J, West R, et al (2016), Deconstructing the alcohol harm paradox: A population based survey of adults in England. PLoS One. 11(9): e0160666. doi:10.1371/journal.pone.0160666
- Beard E, Brown J, West R, Kaner E, Meier P, Michie S (2019), Associations between socio-economic factors and alcohol consumption: A population survey of adults in England. PLoS One. 14(2): e0209442. doi:10.1371/journal.pone.0209442
- Boniface S, Lewer D, Hatch SL, Goodwin L (2020), Associations between interrelated dimensions of socio-economic status, higher risk drinking and mental health in South East London: A cross-sectional study. PLoS One. 15(2): e0229093. doi:10.1371/journal.pone.0229093
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J (2009), Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 373(9682): 2223-2233. doi:10.1016/S0140-6736(09)60746-7
- Estimating the Costs of Health Inequalities: A Report Prepared for the Marmot Review (2010), Frontier Economics
- Marmot M (2010)
- Lorenc T, Petticrew M, Welch V, Tugwell P (2013), What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 67(2): 190-193. doi:10.1136/jech-2012-201257
- Marmot M (2010)
- Public Health England (August 2019), Public Health Outcomes Framework 2019–2022
- Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J (2020) Health Equity in England: The Marmot Review 10 Years On
- Probst C, Roerecke M, Behrendt S, Rehm J (2014)
- Rehm J, Probst C (2018), Decreases of Life Expectancy Despite Decreases in Non-Communicable Disease Mortality: The Role of Substance Use and Socioeconomic Status. Eur Addict Res. 24(2): 53-59. doi:10.1159/000488328
- Probst C, Kilian C, Sanchez S, Lange S, Rehm J (2020), The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: a systematic review. Lancet Public Health. 5(6): e324-e332. doi:10.1016/S2468-2667(20)30052-9
- Rehm J (2011), The risks associated with alcohol use and alcoholism. Alcohol Res Health. 34(2): 135-143
- Lewer D, Jayatunga W, Aldridge RW, et al (2020), Premature mortality attributable to socioeconomic inequality in England between 2003 and 2018: an observational study. Lancet Public Health. 5(1): e33-e41. doi:10.1016/S2468-2667(19)30219-1
- Bellis MA, Hughes K, Wood S, Wyke S, Perkins C (2011), National five-year examination of inequalities and trends in emergency hospital admission for violence across England. Inj Prev. 17(5): 319-325. doi:10.1136/ip.2010.030486
- Long SJ, Fone D, Gartner A, Bellis MA (2016), Demographic and socioeconomic inequalities in the risk of emergency hospital admission for violence: cross-sectional analysis of a national database in Wales. BMJ Open. 6(8): e011169. doi:10.1136/bmjopen-2016-011169
- Bellis MA, Hughes K, Wood S, Wyke S, Perkins C (2011), National five-year examination of inequalities and trends in emergency hospital admission for violence across England
- World Health Organization. Global Status Report on Alcohol and Health 2018. World Health Organization; 2018
- Bryant L (2020), Inequalities in Victimisation: Alcohol, Violence, and Anti-Social Behaviour. Institute of Alcohol Studies
- Bryant L (2020), Inequalities in Victimisation: Alcohol, Violence, and Anti-Social Behaviour
- World Health Organization (2012), Understanding and Addressing Violence against Women
- Reichel D (2017), Determinants of intimate partner violence in europe: the role of socioeconomic status, inequality, and partner behavior. J Interpers Violence. 32(12): 1853-1873. doi:10.1177/0886260517698951
- Bryant L (2020)
- Bryant L (2020)
- Gell L, Ally A, Buykx P, Hope A, Meier P (2015), Alcohol’s Harm to Others. Institute of Alcohol Studies
- Ransome Y, Luan H, Shi X, Duncan DT, Subramanian SV (2019), Alcohol Outlet Density and Area-Level Heavy Drinking Are Independent Risk Factors for Higher Alcohol-Related Complaints. J Urban Health. 96(6): 889-901. doi:10.1007/s11524-018-00327-z
- Buckner JC (2008), Understanding the Impact of Homelessness on Children: Challenges and Future Research Directions. American Behavioral Scientist. 51(6): 721-736. doi:10.1177/0002764207311984
- Alcohol Research UK (2015), Understanding the Alcohol Harm Paradox in Order to Focus the Development of Interventions
- Mabhala MA, Yohannes A, Griffith M (2017), Social conditions of becoming homelessness: qualitative analysis of life stories of homeless peoples. Int J Equity Health. 16(1): 150. doi:10.1186/s12939-017-0646-3
- May PA, Gossage JP (2011), Maternal risk factors for fetal alcohol spectrum disorders: not as simple as it might seem. Alcohol Res Health. 34(1): 15-26
- May PA, Gossage JP (2011), Maternal risk factors for fetal alcohol spectrum disorders: not as simple as it might seem
- Meurk C, Lucke J, Hall W (2014), A Bio-Social and Ethical Framework for Understanding Fetal Alcohol Spectrum Disorders. Neuroethics. 7(3): 337-344. doi:10.1007/s12152-014-9207-2
- Singal D, Brownell M, Wall-Wieler E, et al (2019), Prenatal care of women who give birth to children with fetal alcohol spectrum disorder in a universal health care system: a case-control study using linked administrative data. CMAJ Open. 7(1): E63-E72. doi:10.9778/cmajo.20180027
- Pfinder M, Liebig S, Feldmann R (2012), Explanation of social inequalities in hyperactivity/inattention in children with prenatal alcohol exposure. Klin Padiatr. 224(5): 303-308. doi:10.1055/s-0032-1314841
- Gauffin K, Hemmingsson T, Hjern A (2013), The effect of childhood socioeconomic position on alcohol-related disorders later in life: a Swedish national cohort study. J Epidemiol Community Health. 67(11): 932-938. doi:10.1136/jech-2013-202624
- Sadler S, Angus C, Gavens L, et al (2017), Understanding the alcohol harm paradox: an analysis of sex- and condition-specific hospital admissions by socio-economic group for alcohol-associated conditions in England. Addiction. 112(5): 808-817. doi:10.1111/add.13726
- Green MA, Strong M, Conway L, Maheswaran R (2017), Trends in alcohol-related admissions to hospital by age, sex and socioeconomic deprivation in England, 2002/03 to 2013/14. BMC Public Health. 17(1): 412. doi:10.1186/s12889-017-4265-0
- Jones L, Bates G, McCoy E, Bellis MA (2015), Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis
- Hashibe M, Brennan P, Benhamou S, et al (2007), Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J Natl Cancer Inst. 99(10): 777-789. doi:10.1093/jnci/djk179
- Islami F, Tramacere I, Rota M, et al (2010), Alcohol drinking and laryngeal cancer: overall and dose-risk relation–a systematic review and meta-analysis. Oral Oncol. 46(11): 802-810. doi:10.1016/j.oraloncology.2010.07.015
- Conway DI, Petticrew M, Marlborough H, Berthiller J, Hashibe M, Macpherson LMD (2008), Socioeconomic inequalities and oral cancer risk: a systematic review and meta-analysis of case-control studies
- Menvielle G, Kunst AE, Stirbu I, et al (2007), Socioeconomic inequalities in alcohol related cancer mortality among men: to what extent do they differ between Western European populations? Int J Cancer. 121(3): 649-655. doi:10.1002/ijc.22721
- Bryant L (2020)
- Local Alcohol Profiles for England (2020) Public Health Profiles
- Warburton AL, Shepherd JP (2002), Alcohol-related violence and the role of oral and maxillofacial surgeons in multi-agency prevention. Int J Oral Maxillofac Surg. 31(6): 657-663. doi:10.1054/ijom.2002.0245
- Conway DI, McMahon AD, Graham L, et al (2010), The scar on the face of Scotland: deprivation and alcohol-related facial injuries in Scotland. J Trauma. 68(3): 644-649. doi:10.1097/TA.0b013e3181a5ed18
- Conway DI, McMahon AD, Graham L, et al (2010), The scar on the face of Scotland: deprivation and alcohol-related facial injuries in Scotland
- Herbert A, Gilbert R, Cottrell D, Li L (2017), Causes of death up to 10 years after admissions to hospitals for self-inflicted, drug-related or alcohol-related, or violent injury during adolescence: a retrospective, nationwide, cohort study. Lancet. 390(10094): 577-587. doi:10.1016/S0140-6736(17)31045-0
- IAS, Alcohol and the prison system (old factsheet). Accessed 25 June, 2020
- Zlodre J, Fazel S (2012), All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health. 102(12): e67-75. doi:10.2105/AJPH.2012.300764
- Binswanger IA, Krueger PM, Steiner JF (2009), Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health. 63(11): 912-919. doi:10.1136/jech.2009.090662
- Chang Z, Lichtenstein P, Larsson H, Fazel S (2015), Substance use disorders, psychiatric disorders, and mortality after release from prison: a nationwide longitudinal cohort study. Lancet Psychiatry. 2(5): 422-430. doi:10.1016/S2215-0366(15)00088-7
- Bellis MA, Lowey H, Hughes K, Deacon L, Stansfield J, Perkins C (2012), Variations in risk and protective factors for life satisfaction and mental wellbeing with deprivation: a cross-sectional study. BMC Public Health. 12:492. doi:10.1186/1471-2458-12-492
- Torikka A, Kaltiala-Heino R, Luukkaala T, Rimpelä A (2017), Trends in Alcohol Use among Adolescents from 2000 to 2011: The Role of Socioeconomic Status and Depression. Alcohol Alcohol. 52(1): 95-103. doi:10.1093/alcalc/agw048
- Seth P, Wingood GM, DiClemente RJ, Robinson LS (2011), Alcohol use as a marker for risky sexual behaviors and biologically confirmed sexually transmitted infections among young adult African-American women. Womens Health Issues. 21(2): 130-135. doi:10.1016/j.whi.2010.10.005
- Probst C, Simbayi LC, Parry CDH, Shuper PA, Rehm J (2017), Alcohol use, socioeconomic status and risk of HIV infections. AIDS Behav. 21(7): 1926-1937. doi:10.1007/s10461-017-1758-x
- Fisher JC, Cook PA, Kapiga SH (2010), Alcohol use before sex and HIV risk: situational characteristics of protected and unprotected encounters among high-risk African women. Sex Transm Dis. 37(9): 571-578. doi:10.1097/OLQ.0b013e3181dbafad
- Rehm J, Probst C, Shield KD, Shuper PA (2017), Does alcohol use have a causal effect on HIV incidence and disease progression? A review of the literature and a modeling strategy for quantifying the effect. Popul Health Metr. 15(1): 4. doi:10.1186/s12963-017-0121-9
- Hendershot CS, Stoner SA, Pantalone DW, Simoni JM (2009), Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 52(2): 180-202. doi:10.1097/QAI.0b013e3181b18b6e
- Fisher JC, Bang H, Kapiga SH (2007), The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis. 34(11): 856-863. doi:10.1097/OLQ.0b013e318067b4fd
- Rehm J, Samokhvalov AV, Neuman MG, et al (2009), The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review. BMC Public Health. 9: 450. doi:10.1186/1471-2458-9-450
- Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M (2009), Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 68(12): 2240-2246. doi:10.1016/j.socscimed.2009.03.041
- Local Alcohol Profiles for England (2020) Public Health Profiles
- Mackenbach JP, Bopp M, Deboosere P, et al (2017), Determinants of the magnitude of socioeconomic inequalities in mortality: A study of 17 European countries. Health Place. 47: 44-53. doi:10.1016/j.healthplace.2017.07.005
- Rehm J, Probst C (2018), Decreases of Life Expectancy Despite Decreases in Non-Communicable Disease Mortality: The Role of Substance Use and Socioeconomic Status
- Probst C, Kilian C, Sanchez S, Lange S, Rehm J (2020) The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: a systematic review
- Public Health England, Health Inequalities Dashboard. Accessed June 25, 2020
- Wilcox HC, Conner KR, Caine ED (2004), Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 76 Suppl: S11-9. doi:10.1016/j.drugalcdep.2004.08.003
- Innamorati M, Lester D, Amore M, Girardi P, Tatarelli R, Pompili M (2010), Alcohol consumption predicts the EU suicide rates in young women aged 15-29 years but not in men: analysis of trends and differences among early and new EU countries since 2004. Alcohol. 44(5): 463-469. doi:10.1016/j.alcohol.2010.07.007
- Mäki N, Martikainen P (2009), The role of socioeconomic indicators on non-alcohol and alcohol-associated suicide mortality among women in Finland. A register-based follow-up study of 12 million person-years. Soc Sci Med. 68(12): 2161-2169. doi:10.1016/j.socscimed.2009.04.006
- Innamorati M, Lester D, Amore M, Girardi P, Tatarelli R, Pompili M (2010), Alcohol consumption predicts the EU suicide rates in young women aged 15-29 years but not in men: analysis of trends and differences among early and new EU countries since 2004
- Office of National Statistics (2013) Trends in All-Cause Mortality by NS-SEC for English Regions and Wales, 2001–03 to 2008–10
- Local Alcohol Profiles for England (2020) Public Health Profiles
- Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J (2020), Health Equity in England: The Marmot Review 10 Years On. Institute of Health Equity
- Probst C, Roerecke M, Behrendt S, Rehm J (2014); Probst C, Kilian C, Sanchez S, Lange S, Rehm J (2020)
- Richardson EA, Hill SE, Mitchell R, Pearce J, Shortt NK (2015), Is local alcohol outlet density related to alcohol-related morbidity and mortality in Scottish cities? Health Place. 33: 172-180. doi:10.1016/j.healthplace.2015.02.014
- Waller MW, Iritani BJ, Christ SL, Tucker Halpern C, Moracco KE, Flewelling RL (2013), Perpetration of intimate partner violence by young adult males: the association with alcohol outlet density and drinking behavior. Health Place. 21:10-19. doi:10.1016/j.healthplace.2013.01.002
- Shortt NK, Rind E, Pearce J, Mitchell R, Curtis S (2018), Alcohol risk environments, vulnerability, and social inequalities in alcohol consumption. Annals of the American Association of Geographers. 108(5): 1-18. doi:10.1080/24694452.2018.1431105
- Alcohol Change UK, Full to the brim? Outlet density and alcohol-related harm. Accessed June 25, 2020
- Grubesic TH, Pridemore WA (2011), Alcohol outlets and clusters of violence. Int J Health Geogr. 10: 30. doi:10.1186/1476-072X-10-30
- Alcohol Outlet Density, Deprivation, and Crime in Scotland. Accessed June 25, 2020
- Richardson EA, Hill SE, Mitchell R, Pearce J, Shortt NK (2015), Is local alcohol outlet density related to alcohol-related morbidity and mortality in Scottish cities? Health Place. 33: 172-180. doi:10.1016/j.healthplace.2015.02.014
- Shortt NK, Rind E, Pearce J, Mitchell R, Curtis S (2018), Alcohol risk environments, vulnerability, and social inequalities in alcohol consumption. Annals of the American Association of Geographers. 108(5): 1-18. doi:10.1080/24694452.2018.1431105
- Lightowlers C, Pina-Sánchez J, McLaughlin F (July 2020), The role of deprivation and alcohol availability in shaping trends in violent crime
- Sharpe CA, Poots AJ, Watt H, Franklin D, Pinder RJ (2018), Controlling alcohol availability through local policy: an observational study to evaluate Cumulative Impact Zones in a London borough. J Public Health. 40(3): e260-e268. doi:10.1093/pubmed/fdx167
- World Health Organization (2018), Global Status Report on Alcohol and Health 2018
- Popova S, Giesbrecht N, Bekmuradov D, Patra J (2009), Hours and days of sale and density of alcohol outlets: impacts on alcohol consumption and damage: a systematic review. Alcohol Alcohol. 44(5): 500-516. doi:10.1093/alcalc/agp054
- Chen M-J, Grube JW, Bersamin M, Waiters E, Keefe DB (2005), Alcohol advertising: what makes it attractive to youth? J Health Commun. 10(6): 553-565. doi:10.1080/10810730500228904
- Roche A, Kostadinov V, Fischer J, et al (2015), Addressing inequities in alcohol consumption and related harms. Health Promot Int. 30 Suppl 2: ii20-35. doi:10.1093/heapro/dav030
- Gentry E, Poirier K, Wilkinson T, Nhean S, Nyborn J, Siegel M (2011), Alcohol advertising at Boston subway stations: an assessment of exposure by race and socioeconomic status. Am J Public Health. 101(10): 1936-1941. doi:10.2105/AJPH.2011.300159
- Hoyos Cillero I, Jago R (2010), Systematic review of correlates of screen-viewing among young children. Prev Med. 51(1): 3-10. doi:10.1016/j.ypmed.2010.04.012
- Purshouse RC, Meier PS, Brennan A, Taylor KB, Rafia R (2010), Estimated effect of alcohol pricing policies on health and health economic outcomes in England: an epidemiological model. Lancet. 375(9723): 1355-1364. doi:10.1016/S0140-6736(10)60058-X
- Page N, Sivarajasingam V, Matthews K, Heravi S, Morgan P, Shepherd J (2017), Preventing violence-related injuries in England and Wales: a panel study examining the impact of on-trade and off-trade alcohol prices. Inj Prev. 23(1): 33-39. doi:10.1136/injuryprev-2015-041884
- O’Donnell A, Anderson P, Jané-Llopis E, Manthey J, Kaner E, Rehm J (2019), Immediate impact of minimum unit pricing on alcohol purchases in Scotland: controlled interrupted time series analysis for 2015-18. BMJ. 366: l5274. doi:10.1136/bmj.l5274
- Bhattacharya A (2020), Who Pays the Tab?: The Distributional Effects of UK Alcohol Taxes. Institute of Alcohol Studies
- Probst C, Roerecke M, Behrendt S, Rehm J (2014)
- The King’s Fund (2012), Health Policy under the Coalition Government
- Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J (2020)
- Marmot M (2010)
View this report
